Dementia .Cognition .Mild cognitive impairment-various aspects-
Overview –
Mild cognitive impairment (MCI) is the stage between the expected age-related decline in memory and thinking and the more severe decline of dementia. MCI can have problems with memory, language, or judgment. People with MCI may be aware that their memory or mental functioning has “slipped.” Family and close friends may also notice changes. But these changes are not bad enough to affect daily life or normal activities.
MCI –Mild cognitive impairment-can increase the risk of dementia due to Alzheimer’s disease or other brain diseases. But some people with mild cognitive impairment may never get worse. And some eventually get better..
Symptoms –
The brain, like the rest of the body, changes with age. Many people find that they become more forgetful as they get older. It may take longer to think of a word or remember a person’s name. If mental health problems are more severe than expected, symptoms may be due to mild cognitive impairment (MCI). MCI can cause changes in thinking if .You forget things more often. You miss meetings or social events.You lose your mind. Or you can’t follow the plot of a book or movie.
You have trouble following a conversation. You have trouble making decisions, completing tasks, or following directions.You begin to have trouble finding familiar places. You have trouble. poor judgment begins. Your family and friends will notice some of these changes.
If you have MCI- mild cognitive impairment you may also experience: Depression. ,Anxiety ,Low mood and aggression ,Lack of interest. .When to See a Neurologist ,Talk with him if you or a loved one notices that you are having problems with your memory or thinking. This can include difficulty remembering recent events or thinking clearly..
Mild cognitive impairment (MCI) has no single cause, although MCI can be caused by early Alzheimer’s disease. An alarm does not have one result. MCI symptoms can remain stable for years. Or MCI can progress to Alzheimer’s dementia or other types of dementia.
In some cases, MCI can improve over time.
MCI –mild cognitive impairment often involves the same types of brain changes as Alzheimer’s disease or other forms of dementia. In MCI, these changes occur to a lesser extent. Some of these changes have been seen in autopsy studies of MCI patients. These changes include-clumps of beta-amyloid protein called plaques and tangles of tau proteins seen in Alzheimer’s disease.
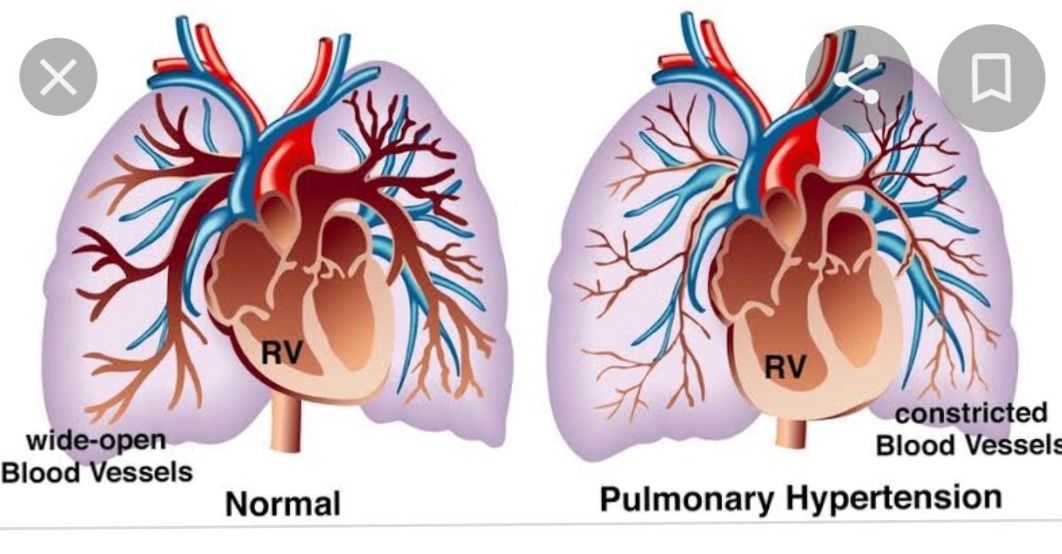
Microscopic lumps -a protein called a Lewy body. Those nodules are associated with Parkinson’s disease, dementia with Lewy bodies and some Alzheimer’s diseases , Small strokes or reduced blood flow to brain vessels.
Brain imaging studies show that the following changes may be associated with MCI – mild cognitive impairment .The size of the hippocampus, an area of the brain important for memory, decreases. The cerebral fluid spaces called ventricles increase.In the central regions of the brain, the use of glucose decreases. Glucose is a sugar that is the main source of energy for cells.
Risk factors –
The strongest risk factors for MCI-mild cognitive impairment are:-
Aging. A form of the gene known as APOE e4.
This gene is also associated with Alzheimer’s disease. But having the gene does not guarantee impaired thinking and memory.
Other diseases and lifestyle factors have been linked to an increased risk of changes in thinking, including:-
Diabetes., Smoking ,High blood pressure .High cholesterol ,Obesity. Depression ,Obstructive sleep apnea. Lack of physical exercise ,Low education, Lack of wellness or socially stimulating activities..
Complications-of Mild cognitive impairment-
Patients with MCI mild cognitive impairment – have an increased risk, but no certainty, of developing dementia. . . In general, approximately 1-3% of older adults develop dementia each year. Studies show that approximately 10-15% of MCI –Mild cognitive impairment patients develop dementia each year.
Prevention -Medical decline in cognitive function cannot be avoided. However, research has shown that certain lifestyle factors can reduce the risk of developing MCI-Mild cognitive impairment -Research shows that these actions can help prevent MCI:
Don’t drink large amounts of alcohol. Limit exposure to air pollution.
Reduce your risk of head injury. Don’t smoke. Manage medical conditions such as diabetes. , high blood pressure, obesity and depression. Practice good sleep hygiene and manage sleep disorders .Eat a healthy diet full of nutrients. Include fruits and vegetables and foods low in saturated fat .Stay with friends and family. Exercise at a moderate to vigorous intensity most days of the week. If you have hearing loss, use a hearing aid. You can refresh your mind. with riddles. , games and memory training..
Summary-of-Dementia .Cognition .Mild cognitive impairment-
Clinicians can diagnose dementia (severe neurocognitive impairment) and mild cognitive impairment (mild neurocognitive impairment) syndromes based on history, examination, and appropriate objective assessments using standard criteria such as DSM-5. They can then diagnose etiological subtypes of these syndromes using standard criteria for each. Brain imaging and biomarkers are gaining ground in the differential diagnosis of various diseases.
Treatment of -of-Dementia .Cognition .Mild cognitive impairment- remains largely symptomatic.
When older patients and their families report symptoms of “memory loss,” experienced clinicians know that these concerns are related to multiple cognitive abilities or general cognitive decline. not just a memory. However, some cognitive slowing is characteristic of normal aging. Therefore, the clinician’s first challenge is to identify clinically significant cognitive changes.
Dementia is usually diagnosed when acquired cognitive impairment has become severe enough to impair social and/or occupational functioning. Mild Cognitive Impairment (MCI) is a state between normal cognition and dementia with fairly preserved functional abilities .
Briefly, a DSM-5 diagnosis of a severe neurocognitive disorder equivalent to dementia requires significant impairment in one or (usually) multiple cognitive domains. The disability must be sufficient to prevent independence in daily activities. A diagnosis of mild neurocognitive impairment corresponding to MCI-mild cognitive impairment is made when there is mild impairment in one or more cognitive areas. Man is still independent in daily activities, although with greater effort. A decline in value should reflect a decline from a previous higher level and should be documented both historically and objectively. Furthermore, cognitive deficits should not appear only in relation to delirium or be better explained by another mental disorder. The second challenge for the clinician is to identify the cause(s) of cognitive impairment, ie. identify its root cause ,etiology
DSM-5 also provides diagnostic criteria for the most common etiological subtypes of neurocognitive disorders in all age groups. Here we focus on neurocognitive disorders in older adults..
The Impact of Dementia ,Neurocognitive disorders, especially severe neurocognitive disorders (dementia), have enormous consequences for individuals, their families, the health care system and the economy. In the United States, Alzheimer’s disease (AD) is a leading cause of death, requiring hospitalization, skilled nursing, and home health care.
The health care costs and informal costs of unpaid care for people with dementia are high and increasing. Caregivers also experience increased emotional distress, depression and health problems. In absolute numbers, an estimated 35.6 million people worldwide had dementia in 2010, and that number is expected to reach 115.4 million by 2050.
Dementia in the population-
The prevalence, which is defined as the number of people affected as a proportion of a given population at a given moment in time, is an index of population burden of disease.
Incidence is the rate of occurrence of a new disease in a given population, ie. the proportion of new cases of the disease in that population during a certain period of time. Therefore, incidence is an index of disease risk in this population. Occurrence is a function of both frequency and duration. Because most dementias cannot be cured, their duration reflects how long people live with their dementia. Thus, the public health burden of dementia depends on both the occurrence of new cases and the survival of those cases after they occur;
Holding incidence constant, prevalence is higher in age groups. Dementia prevalence increases exponentially with age 5 and doubles within five years after age 65. In higher income countries, the prevalence is 5-10%. in people over 65, usually more in women than in men, mainly because women live longer than men.
In the United States, a higher prevalence has been reported among African Americans and Latinos/Hispanics than in non-Hispanic white populations. Global systematic reviews and meta-analyses suggest that the prevalence of dementia is lower in sub-Saharan Africa and higher in Latin America than elsewhere in the world . The prevalence of MCI- mild cognitive impairment is currently difficult to determine because it depends on the precise definitions and subtypes of MCI being studied.
Life expectancy is increasing across the planet, and population aging is accelerating faster in low- and middle-income countries. . -income countries, where the prevalence of dementia is expected to increase. According to new studies, the prevalence may stabilize or even decrease in countries with high incomes.
Incidence-
The incidence of dementia increases steadily until age 85 or 90, after which it continues to increase, but at a slower rate. It is similar in men and women or slightly higher in women. Annual age-adjusted rates ranged from 0.1% at age 60-64 to 8.6% at age 95.5. the onset of the disease depending on the type of statistical analysis performed. Protective factors indicate the opposite. The observed risk factor does not necessarily cause the disease; a protective factor may not prevent disease and will almost certainly not cure disease.
Observed effects may reflect selection or survival biases, or confounding or sometimes reverse causation. They can also depend on the time and duration of exposure to the factor, with middle age often being a critical period.
Demographic risk factors-
Aging is not only the strongest risk factor for dementia, but also the only consistently identified risk factor. after the age of eight. Although prevalence is consistently higher among women, incidence is not;
thus, the higher prevalence may be largely due to the longer life expectancy of women.
Lower education levels were found to be associated with higher prevalence. In the United States, prevalence is elevated among African Americans and Hispanics; Some authors have linked these findings to lower levels of education and higher rates of cardiovascular disease in these populations.
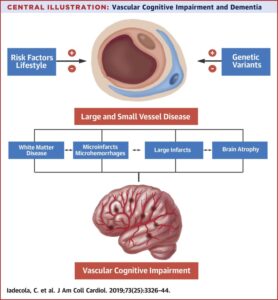
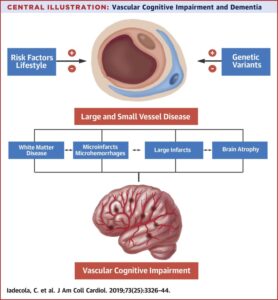
Genetic Factors –Deterministic autosomal dominant genes are responsible for some dementias; these are discussed later under specific disorders. Although several genes have been identified as increasing susceptibility to Alzheimer’s disease, the best established is the Apolipoprotein E (APOE) polymorphism on chromosome 19.
The APOE*4 allele, which is associated with an increased risk of hypercholesterolemia and heart disease, is also associated with dementia .
Dementia with Lewy bodies, vascular dementia and frontotemporal dementia due to Alzheimer’s and Parkinson’s disease in men.
APOE*2 appears to be protective. APOE*4 is a risk factor, not a diagnostic marker for Alzheimer’s disease. It is neither necessary nor sufficient for diagnosis, and its effect on risk appears to decrease by the eighth decade, meaning that individuals over 80 who are APOE*4 positive and do not yet have dementia are not at increased risk of develop dementia. than they are. which , which are APOE*4 negative.
Medical risk factors-for dementia –
Cardiovascular disease is increasingly recognized as not just a risk factor for vascular dementia but also for degenerative dementias, particularly AD. Heart disease has been associated with both dementia of the Alzheimer’s type, and vascular dementia.
Risk factors in midlife, including hypertension, high cholesterol, high body mass index (BMI), and diabetes mellitus are associated with increased risk of dementia in late life, demonstrating the importance of risk exposures decades earlier.
Heart failure and atrial fibrillation are risk factors for cognitive impairment and dementia.
Cardiac disease can cause or worsen cerebral hypoperfusion, creating a cellular energy crisis setting off a cascade of events leading to the production of toxic proteins. In cognitively normal older adults, elevated pulse pressure has recently been found associated with alterations in biomarkers suggestive of AD.3
Inflammation and alterations in inflammatory markers [interleukins, cytokines, C-reactive protein] have been reported in Alzheimer’s and vascular dementias.
Multiple mechanisms have been proposed for the role played by inflammation in the neuropathology of AD.34 35 36Obstructive sleep apnea, associated with hypertension, heart disease, stroke risk37 and white matter change,38 is also associated with an increased risk of dementia. Stroke increases risk of dementia .
Psychiatric risk factors –
Depression has a complex and likely bi-directional association with dementia.
Recurrent major depression in earlier adulthood appears to increase risk of dementia in later life.
Depression with late life onset is believed to be an early sign of the vascular or degenerative disease causing the dementia. Late-life anxiety is associated with cognitive impairment and decline.
Traumatic stress disorder has been reported as increasing risk of dementia.
Head injury- is associated with increased risk of dementia, and the severity of injury appears to heighten this risk. Neurocognitive disorders can occur immediately after a traumatic brain injury or after the recovery of consciousness at any age. However, chronic traumatic encephalopathy (previously termed dementia pugilistica) is diagnosed years after repeated concussive or subconcussive blows to the head, with a clinical presentation similar to AD or frontotemporal lobar degeneration .
Lifestyle and environmental risk factors-
Many environmental and occupational exposures have shown varying associations with neurodegenerative diseases.
Smoking has been associated with an elevated risk of dementia .
Heavy consumption of alcohol increases odds of developing dementia.
Parkinson’s disease risk is associated with exposure to pesticides, for which a molecular mechanism has been established.
Protective factors-for dementia-
Protective factors are factors associated with reduced incidence or likelihood of dementia or delayed onset of dementia.
The concept of “reserve” has been proposed to explain why some people remain cognitively intact despite the presence of neuropathology often associated with dementia.
Brain reserve refers to the structural capacity and integrity of the brain (eg, brain mass, preserved large neurons), while cognitive reserve refers to its functional capacity, especially the ability to use alternative neural networks and compensatory strategies .
Education and Cognitive Functional educational opportunities are universal, higher education may reflect inherent wealth; the training process may also promote reserve development through mechanisms such as increased dendritic branching. Education can also reflect general socioeconomic status and thus the quality of environmental factors such as nutrition or health care. Regardless of the mechanism, higher education is associated with a lower incidence of dementia .
Bilingualism has been associated with late onset of dementia, independent of education, and may protect against declines in attention and executive function .
Cognitive activities: lifelong occupations that do not require higher education or skilled vocational training appear to be associated with a higher risk of dementia.
Several popular leisure activities have been found to be associated with a lower risk of dementia ,appears to have a protective effect for both. and enhance the effect on cognition.
Pharmacological factors -Long-term observational studies have found that the treatment of several other diseases is associated with a decreased risk of dementia. However, these drugs have not been found to prevent dementia in clinical trials. The time and duration of exposure may partially explain these differences, as a protective effect was observed with long-term use several years before the onset of dementia.
Although some studies have found a protective association with nonsteroidal anti-inflammatory drug (NSAID) use, A 2005 meta-analysis found that many of the positive results in the 25 reviewed studies were due to different NSAIDs. biased. Despite conflicting reports on the effect of lipid-lowering HMG Co-A reductase inhibitors (“statins”), the combined results of a recent review and meta-analysis from 2013 suggest a protective effect against dementia.
For estrogen therapy, the WHIMS study did not protect and may have increased the risk of combined hormone therapy in elderly women.
A 2013 meta-analysis of all uses and non-uses concluded that hormones had no effect on dementia.
However, for a long time. -term observational studies suggest that the timing of hormone therapy during menopause may be a critical factor.
Lifestyle factors-
High physical activity is associated with lower risk of neurodegenerative diseases .
Smoking is persistently protective against Parkinson’s disease
Elderly women with a wider social network and who less often participate in mental, social or productive activities showed dementia.
Social, mental and physical lifestyles seem to be important, although reverse causality cannot be excluded. . , because neuropathology often begins decades before symptoms appear..
MEDICAL EVALUATION-
When patients, their family members, or other caregivers voluntarily express worry about cognitive issues, the doctor finds it easier to assess them. In other situations, neither the patient nor the caregiver express concerns, albeit they might if prompted. In the event that the patient disputes any difficulties and there isn’t a trustworthy informant, the clinician may nevertheless notice cognitive impairment; this is more likely to occur when the doctor is familiar with the patient. A patient may occasionally alert the physician or a member of the clinic staff by failing to remember appointments, filling prescriptions, or misinterpreting straightforward instructions. Expert medical professionals can also spot signs of declining cognition in patients who respond vaguely or evasively or who oversimplify little issues.
Is dementia a cognitive impairment?
When acquired cognitive impairment reaches a level that interferes with social and/or vocational functioning, dementia is usually diagnosed. With virtually retained functioning abilities, mild cognitive impairment (MCI) is a state halfway between normal cognition and dementia.
What is the 7 stage of dementia?
Extremely Severe Reduction-
This is crucial since a lot of people can no longer detect when they are thirsty at this point. Alzheimer’s patients require a great deal of assistance from carers at this point in the disease. Despite their best efforts, many families discover that they are unable to care for their loved one at home.
Can you recover from cognitive impairment?
They also show that about 14% to 38% of people with MCI –mild cognitive impairment returned to their normal cognition level. The rate of decline in someone with mild cognitive impairment often depends on the underlying cause. Researchers continue to study the mental and medical changes that occur in people with MCI
How to treat cognitive impairment?
Reading books, learning an instrument, and engaging in other hobbies have all been linked to the preservation of brain function, according to studies. Social interaction can assist maintain mental health and reduce the aging process. It can also make life more fulfilling. Your function may be enhanced by memory training and other cognitive training.
What is cognitive impairment?
Problems relating to a person’s capacity for thought, learning, memory, judgment, and decision-making . Cognitive impairment is characterized by memory loss and difficulties focusing, finishing work, comprehending, remembering, adhering to directions, and problem-solving.
What is cognitive in dementia?
mild impairment of cognitive function. moderate but noticeable memory and thinking issues are described by this term, sometimes known as MCI. Not severe, but mild. Cognitive: relates to how our minds comprehend, plan, and think. Not functioning as well as it should be an impairment.
Can dementia be cured?
Dementia now has no known cure. In actuality, it is unlikely that dementia will ever have a single solution because it is caused by a variety of disorders. The goal of research is to discover treatments for conditions that cause dementia, including frontotemporal dementia, Alzheimer’s disease, and dementia with Lewy bodies.
How long do dementia patients live?
Approximately eight to ten years for Alzheimer’s disease. If a person is diagnosed in their 80s or 90s, their life expectancy is reduced. A small percentage of Alzheimer’s patients have prolonged lifespans—sometimes up to 15 or 20 years. Five years or so for vascular dementia.
What age does dementia start?
Growing older is the biggest known risk factor for dementia, with most instances affecting those 65 years of age and beyond.
What is the best brain supplement for dementia?
Certain supplements are available for purchase to treat dementias such as Alzheimer’s. The most well-known supplements include turmeric, gingko, vitamin E, and omega-3s.
What is the best treatment for dementia?
Handling-
Antagonists of cholinesterase. -These medications function by increasing memantine levels, a chemical messenger implicated in judgment and memory. Memantine, also known as Namenda, functions by controlling glutamate activity.
Other medications. -To treat symptoms or other diseases, you may take additional medications.
What is a quick test for dementia?
The Mini-Cog is a three-minute test that consists of a clock-drawing scoring test and a memory recall test. After a quick training session, it can be used successfully, and a healthcare professional can examine the data to decide whether a full diagnostic assessment is required.
Is cognitive impairment permanent?
Cognitive impairment can be a symptom of an underlying illness rather than being specific to any one disease or condition. Moreover, it is synonymous with “cognitive impairment.” It could be a transient state or a persistent, long-term problem.