Hypertensive kidney disease stage 3-various-aspects-
“Hypertensive kidney disease stage 3” denotes a moderate degree of kidney impairment resulting from elevated blood pressure, where the kidneys are not operating at their best, frequently accompanied by signs such as fatigue, swelling in the extremities, and possible complications including anemia and bone disease; this phase is recognized as “Stage 3 Chronic Kidney Disease (CKD)” and necessitates careful observation and treatment to manage the illness and reduce additional damage.
What is Stage 3 CKD?
In Stage 3 CKD, your kidneys are experiencing mild to moderate damage and are less capable of filtering waste and fluid from your blood. Waste accumulation, or uremia, can occur in your body and result in complications, such as elevated blood pressure, anemia, and issues with your bones.


For update on further important health related topics and frequently asked questions on health topics by general population please click on the link given below to join our WhatsApp group –
https://chat.whatsapp.com/Lv3NbcguOBS5ow6X9DpMMA
Issued in public interest by –
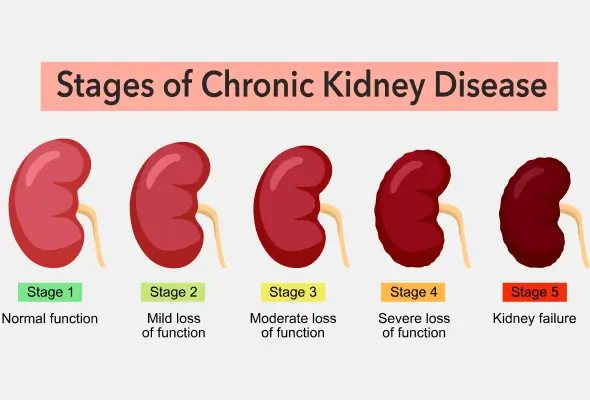
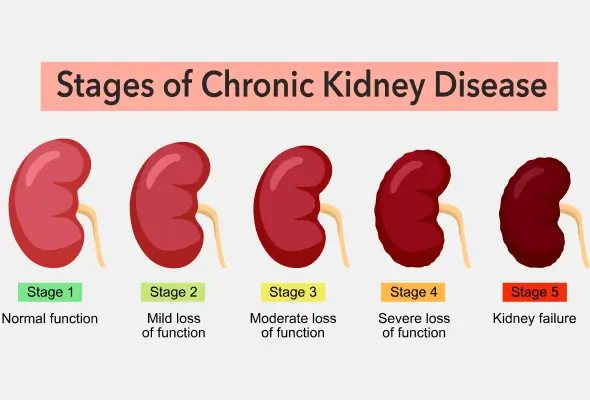
Stage 3 of CKD (eGFR between 30 and 59)
This waste can accumulate in your body and start to lead to additional health issues, such as hypertension and bone disorders. You might start experiencing symptoms like feeling fatigued and weak or having swelling in your hands or feet.


“Hypertensive kidney disease stage 3” denotes a moderate degree of kidney damage due to high blood pressure, where the kidneys are not operating at their best, often presenting symptoms such as fatigue, swelling in the hands and feet, and possible complications like anemia, necessitating close observation and management by a healthcare provider; fundamentally, it represents stage 3 chronic kidney disease (CKD) specifically resulting from hypertension as the main cause.
If any patient of ENT requires any surgery, opd consultation or online consultation in clinic of ENT specialist Doctor Dr Sagar Rajkuwar ,he may contact him at the following address-
Prabha ENT clinic, plot no 345,Saigram colony, opposite Indoline furniture Ambad link road, Ambad ,1 km from Pathardi phata Nashik ,422010, Maharashtra, India-Dr Sagar Rajkuwar (MS-ENT), Cell no- 7387590194 , 9892596635
Key points regarding stage 3 hypertensive kidney disease:
Kidney function:
In this stage, kidney function is considerably impaired, with an estimated glomerular filtration rate (eGFR) ranging from 30 to 59.
Symptoms:
Patients may face fatigue, swelling in the limbs, reduced urine output, foamy urine, muscle cramps, and possible back pain.
Diagnosis:
Diagnosis entails blood examinations to evaluate creatinine levels and calculate eGFR, in addition to urine analysis.
Treatment for stage 3 hypertensive kidney disease:
Blood pressure control:
Rigorous management of high blood pressure using medications such as ACE inhibitors and ARBs is essential to minimize additional kidney damage.
Dietary modifications:
A low-sodium diet, restricting protein consumption based on personal requirements, and controlling fluid intake are vital.
Lifestyle changes:
Engaging in regular exercise, maintaining a healthy weight, and quitting smoking.
Monitoring:
Consistent follow-up with a healthcare provider to track kidney functionality and modify treatment as needed.
Stage 3 CKD is divided into two sub-stages according to your eGFR:
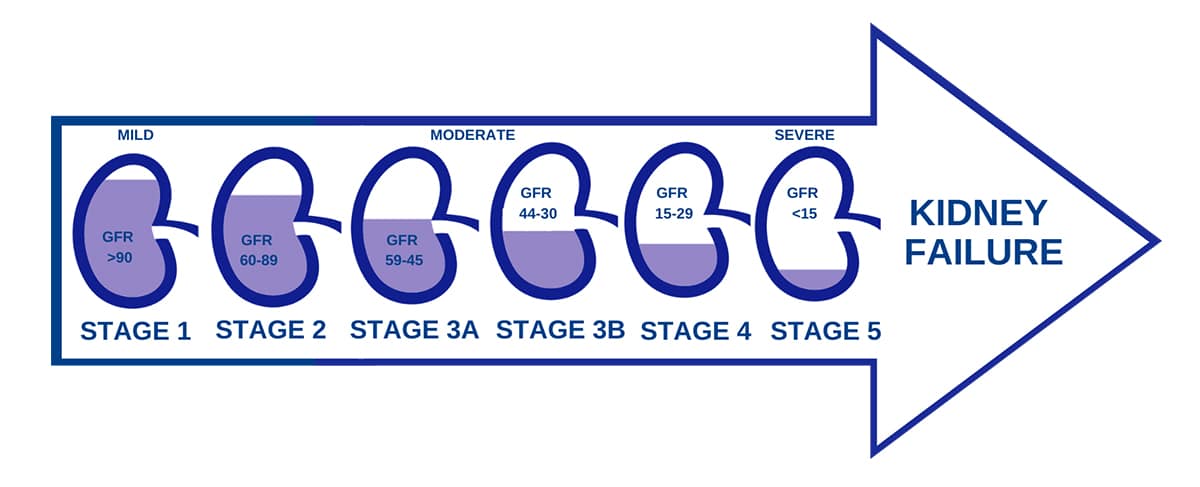
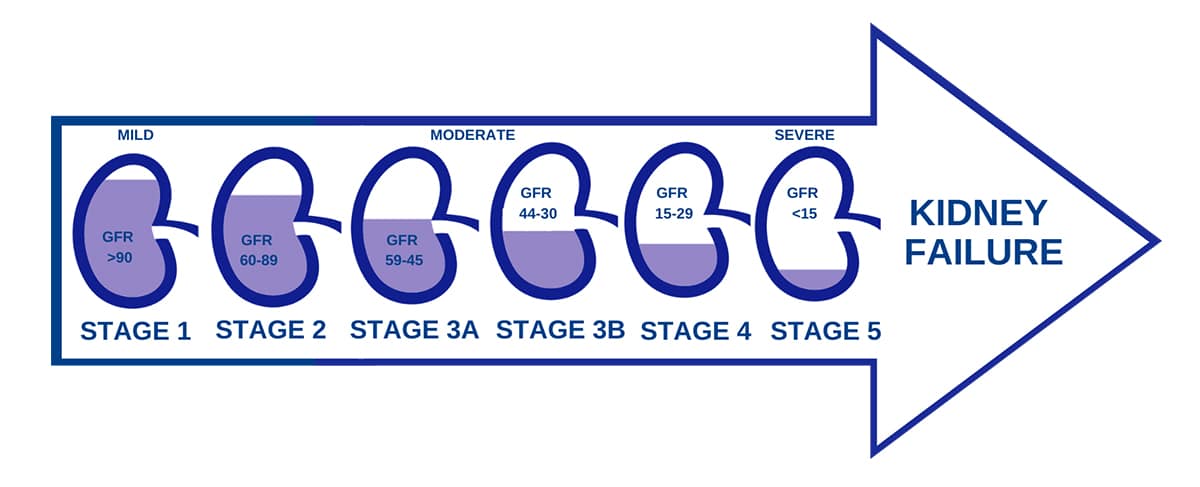
Stage 3a indicates you have an eGFR ranging from 45 to 59.
Stage 3b indicates you have an eGFR between 30 and 44.
How serious is Stage 3 CKD?
Consider Stage 3 CKD as the “middle stage” of kidney disease. Your kidneys are compromised, yet you do not require dialysis or a kidney transplant. During this stage, it’s crucial to monitor not only your kidney function but also the albumin levels in your urine, evaluated through the urine albumin-to-creatinine ratio (uACR). This examination assists in determining if your kidneys are filtering properly. A higher uACR stage signifies that more albumin is present in your urine, which suggests more serious kidney damage.
The higher your uACR stage, the greater your likelihood of kidney disease advancement and complications such as heart disease. Knowing your albumin levels, in conjunction with your eGFR, enables you and your doctor to devise the most effective plan for managing your kidney health and mitigating future risks.
Although there is currently no cure for CKD, and kidney damage is generally not reversible, with treatment, healthy lifestyle modifications, and monitoring your eGFR and uACR, many individuals in Stage 3 do not progress to Stage 4 or Stage 5 (kidney failure).
What are the symptoms of Stage 3 CKD?
Some individuals with Stage 3 CKD exhibit no symptoms. Nevertheless, stage 3 is typically the point at which kidney disease starts to influence your health, and you’ll begin to observe symptoms. It is crucial to keep in mind that even in the absence of symptoms, consistent monitoring is essential for early identification. If you’re classified as high-risk for kidney disease — such as having diabetes, high blood pressure, or a family history of kidney disease — your physician might suggest more frequent assessments to help monitor your kidney health.

Symptoms of Stage 3 CKD may include:
Feeling weak and tired
Swelling in your hands or feet
Skin that feels dry or itchy
Pain in your lower back
Muscle cramps
Trouble sleeping
Restless leg syndrome (an uncomfortable feeling in your legs that makes it hard to sit still or fall asleep)
Urinating more or less often than normal
Urine that is foamy or darker in color than usual
How can doctors tell my stage of CKD?
Your physician might assess your kidney health even in the absence of symptoms if you possess a family history of kidney illness or a medical condition that could harm your kidneys, like diabetes or hypertension.
To determine your stage of CKD, physicians will perform tests, such as:
eGFR blood tests
Urine tests
For Stage 3 CKD, yearly examinations are crucial to gauge the functionality of your kidneys, review your treatment strategy, look for indications of complications, and verify that you are managing your condition properly.
How can doctors tell what caused my CKD?
To discover the cause of your CKD, your doctor may perform other tests, including:
Blood pressure assessments
Urine examinations
Imaging procedures to capture detailed images of the inside of your body, such as ultrasound, CT scan, or MRI
Kidney biopsy (a process where doctors extract a small sample of tissue from your kidneys to examine it under a microscope)
Genetic testing (if doctors have a suspicion of a rare disease or one that is hereditary)
For Stage 3 CKD, yearly checkups are essential to assess the functionality of your kidneys, re-evaluate your treatment strategy, monitor for signs of complications, and ensure you manage your condition effectively.
Comprehending the source of your kidney disease is a crucial step in managing your health. Do not hesitate to inquire with your doctor about the underlying causes of your condition.
Inquire whether further tests are needed to ascertain the root cause or to better understand your kidney function. Be proactive, take control of your health, and make knowledgeable choices regarding your care.
How do doctors treat Stage 3 CKD?
Doctors manage Stage 3 CKD with medications that assist with your symptoms and associated health issues, such as diabetes and high blood pressure.
These medications consist of:
Blood pressure medications like ACE inhibitors and ARBs (even if you do not have high blood pressure, these medications can assist in slowing the damage to your kidneys to maintain their function for as long as possible)
Diabetes medications to maintain your blood sugar at a healthy level (even if you do not have diabetes)
Calcium and vitamin D supplements to support your bones’ strength
Diuretics to assist with swelling (these are medications that help your kidneys eliminate salt and water and increase urination)
Iron supplements to alleviate anemia (not having enough red blood cells in your body)
SGLT2 inhibitors to protect your kidneys and reduce blood sugar levels
Nonsteroidal mineralocorticoid receptor antagonists (nMRA) to decrease swelling and help prevent additional kidney damage
You may also need to discontinue certain medications that can exacerbate damage to your kidneys, such as pain relievers known as NSAIDs (nonsteroidal anti-inflammatory drugs) and some arthritis medications. Inform your doctor about all the medications you take—even those they did not prescribe.
If you do not have a nephrologist (kidney specialist), consult your primary doctor about locating one. You and your nephrologist can collaborate to create a treatment plan tailored specifically for you.
Your nephrologist will also conduct tests to monitor your kidney health regularly, usually every three months.
Issued in public interest by –



