Effects Of Diabetes On Vision-various aspects-
Diabetes affects a person’s eyes when the blood sugar level in the body is high. There are mainly two types of effects of diabetes on the eyes. The first is the short term effect and the second is the long term effect. In the short term, high diabetes levels cause loss of vision. In some situations, individuals have blurred vision for a few days or even a few weeks. When glucose levels in the body are high, it alters the fluid levels in the eyes. As a result it causes inflammation in the eye tissue. The problem of blurred vision is temporary in nature and can be resolved when the glucose level in the body is brought back to normal. Some diseases caused due to high sugar levels in the body are cataract, glaucoma and retinopathy. Diabetes is a major cause of blindness in people between the age range of 20-74.
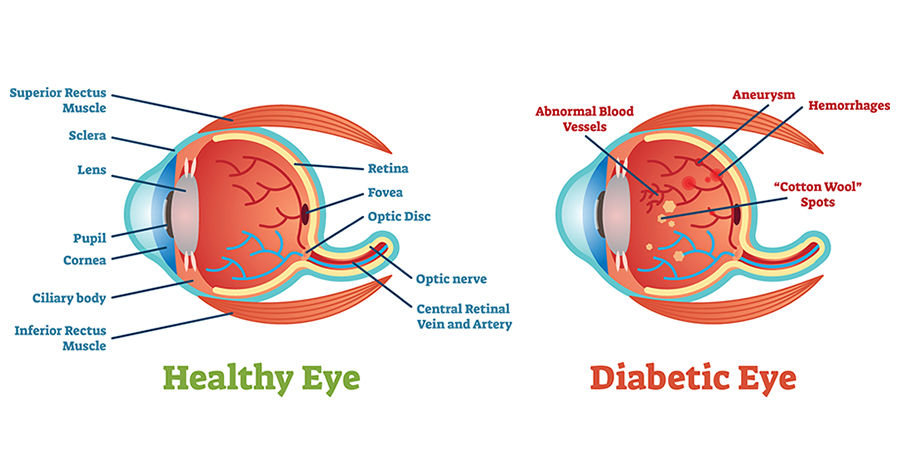
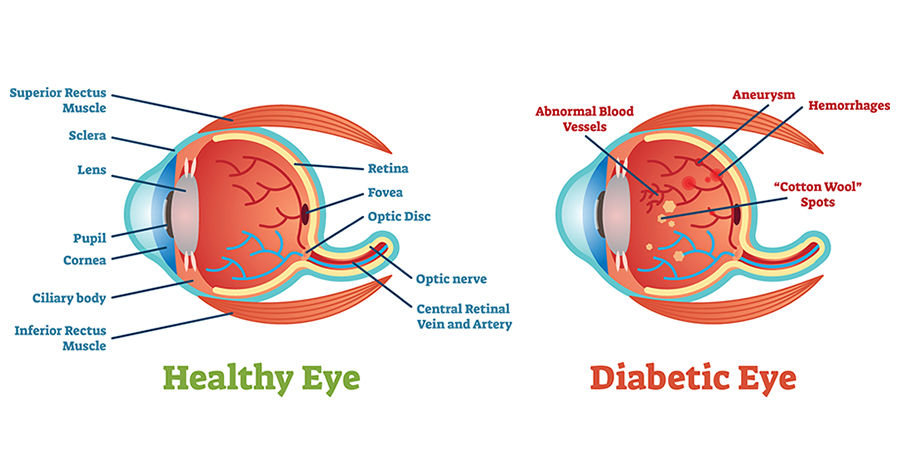
Diabetes can greatly influence vision by leading to a condition known as diabetic retinopathy, where elevated blood sugar harms the blood vessels in the retina, resulting in blurred vision, floaters, and possible vision loss or blindness if not treated; additional eye complications include macular edema, cataracts, and a heightened risk of glaucoma, all of which may affect visual clarity.
Key points regarding diabetes and vision:
Diabetic retinopathy:
The main eye issue associated with diabetes, resulting in damage to the blood vessels of the retina, which can potentially cause vision loss or blindness if not controlled.
Macular edema:
Inflammation in the macula (central region of the retina) that can lead to blurred or distorted vision.
Cataracts:
A clouding of the lens of the eye, which occurs more frequently in individuals with diabetes.
Glaucoma:
Elevated ocular pressure due to impaired blood vessels can result in glaucoma, a condition that affects the optic nerve.
Blurred vision:
A frequent symptom of eye problems related to diabetes, often triggered by changes in blood sugar levels.
Floaters:
Tiny dots or specks that appear in the field of vision, which may indicate diabetic retinopathy.
Important factors to keep in mind:
Blood sugar control:
Ensuring consistent blood sugar levels is essential to avert or slow the advancement of diabetic eye issues.
Regular eye exams:
Individuals with diabetes should undergo regular eye assessments to identify early indicators of eye damage.
Early diagnosis and treatment:
Timely identification and intervention of diabetic eye conditions can assist in protecting vision.
Diabetic retinopathy (DR) is the primary reason for blindness among adults of working age. DR occurs when elevated blood sugar levels harm the blood vessels in the retina (a component of your eye). The affected blood vessels may become swollen and leak, resulting in blurred vision.
What is diabetic retinopathy?
Diabetic retinopathy is an eye disorder that can lead to vision impairment and blindness in individuals with diabetes. It impacts the blood vessels in the retina (the light-sensitive layer of tissue located at the back of your eye).
If you have diabetes, it’s essential to undergo a comprehensive dilated eye examination at least annually. Diabetic retinopathy might not display any symptoms initially — however, detecting it early can assist you in taking measures to safeguard your vision.
Controlling your diabetes — through regular physical activity, a nutritious diet, and adherence to your medication — can also aid in preventing or postponing vision loss.
What are the signs of diabetic retinopathy?
The initial phases of diabetic retinopathy typically do not present any signs. Some individuals observe alterations in their vision, such as difficulty reading or viewing distant objects. These alterations may appear and subside sporadically.
In the more advanced stages of the condition, blood vessels within the retina may begin to bleed into the vitreous (a gel-like substance that occupies your eye). If this occurs, you might notice dark, floating dots or lines resembling cobwebs. Occasionally, the dots may resolve on their own — but seeking treatment promptly is crucial. Without intervention, scars can develop in the rear part of the eye. Blood vessels might also resume bleeding, or the bleeding could intensify.
What additional issues can diabetic retinopathy lead to?
Diabetic retinopathy can result in other severe ocular conditions:
Diabetic macular edema (DME). Over time, approximately 1 in 15 individuals with diabetes will experience DME. DME occurs when retinal blood vessels leak fluid into the macula (a region of the retina essential for clear, central vision). This leads to blurred vision.
Neovascular glaucoma. Diabetic retinopathy can induce the abnormal growth of blood vessels from the retina, obstructing fluid drainage from the eye. This results in a form of glaucoma (a category of eye disorders that may cause vision impairment and blindness).
Retinal detachment. Diabetic retinopathy may lead to scar tissue forming at the back of your eye. When this scar tissue pulls your retina away from the rear of your eye, it is identified as tractional retinal detachment.
Am I susceptible to diabetic retinopathy?
Anyone with any type of diabetes can develop diabetic retinopathy — this includes individuals with type 1, type 2, and gestational diabetes (a form of diabetes that may occur during pregnancy).
Your risk grows the longer you have diabetes. Over time, more than half of those with diabetes will develop diabetic retinopathy. The positive aspect is that you can reduce your chances of developing diabetic retinopathy by managing your diabetes effectively.
Women with diabetes who become pregnant — or those who develop gestational diabetes — are at a heightened risk for developing diabetic retinopathy. If you have diabetes and are expecting, schedule a comprehensive dilated eye exam as soon as possible. Inquire with your doctor whether you will require further eye exams throughout your pregnancy.
What leads to diabetic retinopathy?
Diabetic retinopathy is a result of elevated blood sugar levels due to diabetes. Over time, excessive sugar in your bloodstream can harm your retina — the section of your eye responsible for detecting light and transmitting signals to your brain via a nerve located at the back of your eye (optic nerve).
Diabetes harms blood vessels throughout the body. The harm to your eyesight begins when the glucose in your bloodstream triggers alterations in the small blood vessels leading to your retina. These alterations hinder the blood flow, resulting in blocked blood vessels that either leak fluid or bleed. In response to these obstructed blood vessels, your eyes then develop new blood vessels that function poorly. These new blood vessels are prone to leaking or bleeding easily.
How will my eye doctor check for diabetic retinopathy?
Eye doctors can assess for diabetic retinopathy during a dilated eye examination. The examination is straightforward and painless — your doctor will administer eye drops to dilate (widen) your pupil and then examine your eyes for diabetic retinopathy and other vision issues.
If you suffer from diabetes, it is crucial to have regular eye examinations. Should you develop diabetic retinopathy, early intervention can halt the damage and avert blindness.
If your eye care provider suspects that you might have severe diabetic retinopathy or diabetic macular edema (DME), they might perform a procedure known as a fluorescein angiogram. This procedure allows the doctor to view images of the blood vessels within your retina.
What steps can I take to prevent diabetic retinopathy?
Controlling your diabetes is the most effective method to reduce your chances of developing diabetic retinopathy. This involves maintaining your blood sugar levels within a healthy range. You can achieve this by engaging in consistent physical activity, consuming a nutritious diet, and meticulously adhering to your physician’s guidelines for your insulin or other diabetes medications.
To verify that your diabetes management plan is effective, you will require a specific laboratory test identified as an A1C test. This test indicates your average blood sugar level over the previous three months. You can collaborate with your physician to establish a personal A1C target. Achieving your A1C target can assist in preventing or managing diabetic retinopathy.
Experiencing high blood pressure or elevated cholesterol levels, in conjunction with diabetes, heightens your risk for diabetic retinopathy. Therefore, managing your blood pressure and cholesterol levels can also aid in reducing your risk of vision impairment.
What are the treatment options for diabetic retinopathy and DME?
During the initial stages of diabetic retinopathy, your eye doctor will likely monitor your eye health. Some individuals with diabetic retinopathy may require a thorough dilated eye examination as frequently as every two to four months.
In later stages, it is vital to initiate treatment immediately—especially if you notice changes in your vision. Although it will not reverse any damage that has occurred to your vision, treatment can prevent further deterioration of your eyesight. Additionally, it is essential to take measures to control your diabetes, blood pressure, and cholesterol levels.
Diagnosis
During your eye examination, your physician will assess how well you can see at a distance. Your physician will also dilate your eyes to examine the retina and blood vessels inside your eyes. If you have DR, your eye physician may wish to monitor your vision more often.
The earlier you receive treatment for DR, the more effective that treatment will be. This is why early diagnosis holds significant importance, even if you have not yet experienced symptoms. You should schedule an eye examination to test for DR as soon as you are diagnosed with type 2 diabetes. For type 1 diabetes, you should arrange for an eye examination within five years of diagnosis.
Contact your eye physician if you observe changes in your vision, particularly sudden changes, such as:
Blurring.
Spots.
Flashes.
Blind spots.
Distortion.
Difficulty reading or performing detailed work.
Treatment
Addressing DR can restore damage to the eye and potentially avert blindness for most individuals. Treatment may commence before your vision is compromised. Available options include:
Laser therapy (laser photocoagulation).
Medications known as VEGF inhibitors or corticosteroids.
Vitrectomy (surgical procedure).
Reattachment of the retina (if the retina is detached).




