Congenital Cataract Treatment In Adults-various aspects-
Treatment for adults with congenital cataracts usually involves surgical removal of the clouded lens and, if the patient is not aphakic (lacking a natural lens), implantation of a clear artificial lens (IOL). The main course of therapy for vision loss brought on by congenital cataracts is cataract surgery.


Elaboration:
Surgical removal:
The typical procedure to remove the hazy lens is cataract surgery, notably extracapsular cataract extraction (ECCE). The lens is removed after the cornea is cut, and an IOL is placed in its place.
Intraocular lens (IOL) implantation:
The key to regaining excellent vision is replacing the native lens with an IOL. There are several different kinds of IOLs, and the selection depends on the surgeon’s choice and the patient’s specific demands.
Postoperative treatment:
Patients may need their vision corrected with glasses or contact lenses after surgery, particularly if the implanted IOL does not completely address their refractive error.
Managing Amblyopia:
If, during childhood, the better-seeing eye is favored in cases of unilateral (one-eye) cataracts, amblyopia (lazy eye) can result. Following cataract surgery, vision therapy may be required to address amblyopia.
Possible Problems:
Retinal detachment, infection, and issues connected to the IOL are just a few of the hazards associated with cataract surgery, as with any surgical procedure.
Medical Treatment:
Medical therapy aimed at preventing and treating amblyopia may be advised in some situations, particularly in conjunction with surgical procedures.
If Any Patient of ENT Requires Any Surgery, Opd Consultation Or Online Consultation In Clinic of ENT Specialist Doctor Dr. Sagar Rajkuwar ,He May Contact Him At The Following Address-
Prabha ENT Clinic, Plot no 345,Saigram Colony, Opposite Indoline Furniture Ambad Link Road ,Ambad ,1 km From Pathardi Phata Nashik ,422010 ,Maharashtra, India-Dr. Sagar Rajkuwar (MS-ENT), Cell No- 7387590194, 9892596635
Treatment
Is there a remedy?
Congenital cataracts are treated over a lengthy period of time that demands a lot of parental commitment and effort. A combination of the following is included:
- A surgical operation known as cataract surgery is used to remove the cataract. It may include the insertion of a clear artificial lens, known as an intraocular lens (IOL).
- Regular visual monitoring following surgery or if it is not performed
- Patching the stronger eye to encourage visual development in the weaker eye (occlusion therapy).
- Glasses/contact lenses
Does my Husband need surgery?
Surgery is not necessary if the cataract is not interfering with the development of vision. Routine vision monitoring is often enough to ensure that it is not deteriorating. If the afflicted eye is getting weaker but not to the point where surgery is necessary, occlusion therapy may be necessary in some cases.


Surgery for cataracts is advised if the condition severely impairs eyesight. Surgery is often carried out between the ages of 6 and 8 weeks if the cataract is present from birth, since there is a greater chance of problems if performed earlier. [6-8] The operation is performed under general anaesthesia, so the youngster will be unconscious throughout. Surgery for youngsters with bilateral cataracts is performed one eye at a time.
The eye loses its ability to focus when the natural lens (which is impacted by cataract) is surgically removed. There are two ways to deal with this:
- Putting in an IOL during the procedure
- Using contact lenses or glasses to aid with focusing while leaving the eye without a lens (aphakia)
In order to choose between the two alternatives, a number of variables must be taken into account. The ophthalmologist who is caring for your child will talk with you about the potential advantages and disadvantages of each choice, as well as the procedure itself.
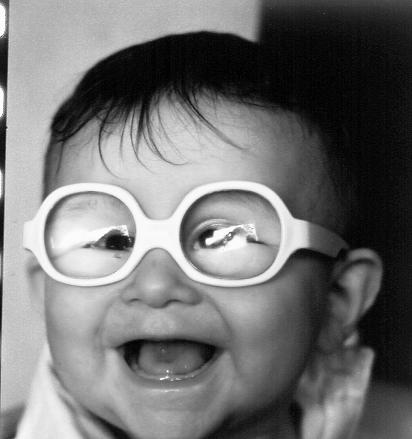
In general, children under the age of two are kept aphakic since IOL implantation in this age group carries a higher risk of complications without providing any additional advantages for visual improvement. At a later age, an IOL implant can be implanted in aphakic children during a subsequent procedure.
What might happen after surgery?
The following problems may develop following surgery:
- Opacification of the visual axis: This is a frequent side effect of cataract surgery in youngsters. It happens when the remaining lens cells begin to accumulate and create a membrane over the lens capsule, also known as the “pocket” where the natural lens sits. Consequently, vision may blur once more due to the diminished amount of light that can pass through. If vision is severely impaired, additional surgery may be necessary. Children who are implanted with an IOL before the age of two are more at risk.
- Glaucoma—This ailment can strike children who have undergone surgery for congenital cataracts; continuous observation is necessary.
- The natural lens can change its form to focus clearly on both close and distant objects, but it cannot concentrate on close objects like a book (accommodation). The natural lens is removed, and this skill is lost. The child may still need contact lenses or glasses to aid in focusing on nearby objects, even with an IOL implant, as the implanted IOL can only focus on distant objects.
- Retinal detachment
- Eye illness (uncommon)
For Update On Further Important Health Related Topics And Frequently Asked Questions On Health Topics By General Population Please Click On The Link Given Below To Join Our WhatsApp Group –
https://chat.whatsapp.com/Lv3NbcguOBS5ow6X9DpMMA
Post-operative visual restoration
Visual gain cannot be assured by the procedure alone. In order to obtain the greatest potential long-term outcome, many procedures are carried out to optimize the development of the visual pathway in the treated eye. These often include:
- Consistent monitoring of visual function and other related eye disorders, such as glaucoma, that will need therapy
- As necessary, update the prescription for glasses or contact lenses. At first, this may happen rather often as the child’s eye is still growing, but it will usually stabilize with age.
- Occlusion treatment involves patching the stronger eye for a few hours each day to promote the weaker eye. The child and the parents typically go through a lengthy and rigorous procedure. In the long run, strict adherence improves the chance of attaining a superior aesthetic result, even if some kids may require ongoing encouragement.
The amount of visual improvement varies from person to person and is influenced by a number of variables, such as:
- When the cataract is discovered (i.e., earlier detection leads to earlier treatment)
- If there are other medical and/or ocular ailments that occur simultaneously
- Any issues occurring either during or after surgery
- Adherence to occlusion treatment
Children who undergo surgery for bilateral cataracts tend to have better vision than those with unilateral cataracts. However, despite rehabilitation efforts, the vision in the operated eye(s) is still often impaired, with only a quarter or less of patients in the UK reaching the bare minimum requirements for driving.
Systemic administration
Due to the complexity of children with syndromic cataracts, a multidisciplinary strategy involving many specialists is advised. The many specialties involved may be coordinated by pediatricians, who can also create suitable treatment routes, such as community-based care.
Early visual impairment can have a detrimental effect on a child’s overall development. As a result, it is essential to make a timely referral to professionals who are knowledgeable about developmental surveillance and intervention for youngsters with visual impairment (VI), such as developmental pediatricians and a Qualified Teacher of children and young people with Visual Impairment (QTVI), in order to maximize their developmental potential.
From infancy to age three, the Developmental Journal for Infants and Young Children with Visual Impairment (DJVI) monitors development and visual advancement using a systematic early intervention curriculum. In collaboration with the child’s parents, it is often used by licensed healthcare providers who treat infants and young children with VI in support services. Children with VI can be recommended to specialized services for additional care, such as the developmental vision clinic at Great Ormond Street Hospital for Children or other specialized developmental services.
FOR INFORMATION IN GREAT DETAIL ON Cataract meaning PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Cataract Surgery PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON What are the 3 types of cataract surgery PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON How long to wear eye shield at night after cataract surgery PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Cataract Symptoms PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Cortical cataract PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Cataract Surgery Recovery Time PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Difference between glaucoma and cataract PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Congenital Cataract PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON What are the disadvantages of cataract surgery PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
If Any Patient of ENT Requires Any Surgery, Opd Consultation Or Online Consultation In Clinic of ENT Specialist Doctor Dr. Sagar Rajkuwar ,He May Contact Him At The Following Address-
Prabha ENT Clinic, Plot no 345,Saigram Colony, Opposite Indoline Furniture Ambad Link Road ,Ambad ,1 km From Pathardi Phata Nashik ,422010 ,Maharashtra, India-Dr. Sagar Rajkuwar (MS-ENT), Cell No- 7387590194, 9892596635
Issued In Public Interest By –
www.entspecialistinnashik.com
Surgery for Congenital Cataract
Introduction
The treatment of a common age-related cataract differs significantly from the management of a congenital cataract. In adults, surgery may be postponed for several years without impacting the visual result. In infants, vision will never be fully restored after surgery if the cataract is not removed during the first year of life. If the aphakia is not treated in adults right away, it can be treated at a later time. If the aphakia is not treated in young children, the vision will never develop properly.
Preoperative Assessment
The pre-operative evaluation is critical because treating a congenital cataract is a far more complicated procedure. We are aware that the majority of negative outcomes in adults following cataract surgery are caused by improper case selection. A wrong judgment at this point might lead to youngsters being blind for the remainder of their lives.
The child’s immediate family is also impacted by congenital cataracts. The funds used for treatment mean that there is less money available to support the education of other kids. The family will be responsible for carrying out the majority of the treatment, so it is imperative that they comprehend the prognosis and length of treatment. In order to care for their own kids, the families must become our partners and colleagues.
Investigations
Age-related cataracts typically occur in isolation, and we seldom examine patients in order to determine the underlying cause of their lens opacity. In children, though, cataract is far less prevalent and more likely to be related to a systemic ailment. In childhood, cataract may be linked to a variety of diseases (Box 1). The majority of these are uncommon, and the etiology of the cataract is unknown in many youngsters. The majority of cataracts in children in affluent nations, with practically infinite resources, have no known cause.
Performing several tests and investigations on every child with cataracts is not beneficial. It is preferable to get a comprehensive history from the parents, including a family history. Inquire about any ailments or medications that were taken throughout the pregnancy, and check to see that the baby is growing as expected. Keep in mind that every blind child will have some developmental lag, which typically goes away if vision is restored. But speaking and hearing should progress at a typical rate.
If at all feasible, a pediatrician should evaluate the kid to check for additional birth defects and assess whether they are healthy enough to undergo general anesthesia. Further investigation is pointless if the history and examination do not provide any insights into the reason of the cataract.
When to perform the surgery
Operating on cataract follows a straightforward set of guidelines. The only time when cataracts should be removed is when
- They are impeding one’s ability to live a decent life.
- Surgery has a fair chance of greatly enhancing eyesight.
This is also the case for cataracts acquired at birth. Unfortunately, it might be quite hard to get kids to respond to these two queries. In general, if a child is behaving and growing normally, don’t operate, but keep monitoring. The demands on the eyes will rise as the youngster gets older. For instance, a slight cataract may not prevent a four-year-old child from playing outside, but it may make it difficult for him to learn to read at school when he is six or seven. The red reflex can be deceptive since youngsters can have excellent vision even when the red reflex cannot be seen via a zonular cataract. Keep in mind that a child’s capacity to accommodate is lost when a cataract is removed. They might be better off with 6/18 and a full range of lodging options than they would be with 6/9 and no depth of field.
Even though pediatric cataract surgery should be performed as soon as possible, children are unlikely to be severely harmed if they wait a bit longer if there is legitimate question as to whether they will benefit. It gets simpler to examine their eyesight and decide if they require surgery as they get older.
Surgery
Children undergo cataract surgery that is quite different from that for adults. General anesthesia will be necessary for the procedure. Associated cardiac or other birth defects may exist. The behavior of an infant’s eye is quite different from that of an adult’s. Surgery for congenital cataracts should only be performed in facilities that are adequately prepared to handle these complicated procedures.
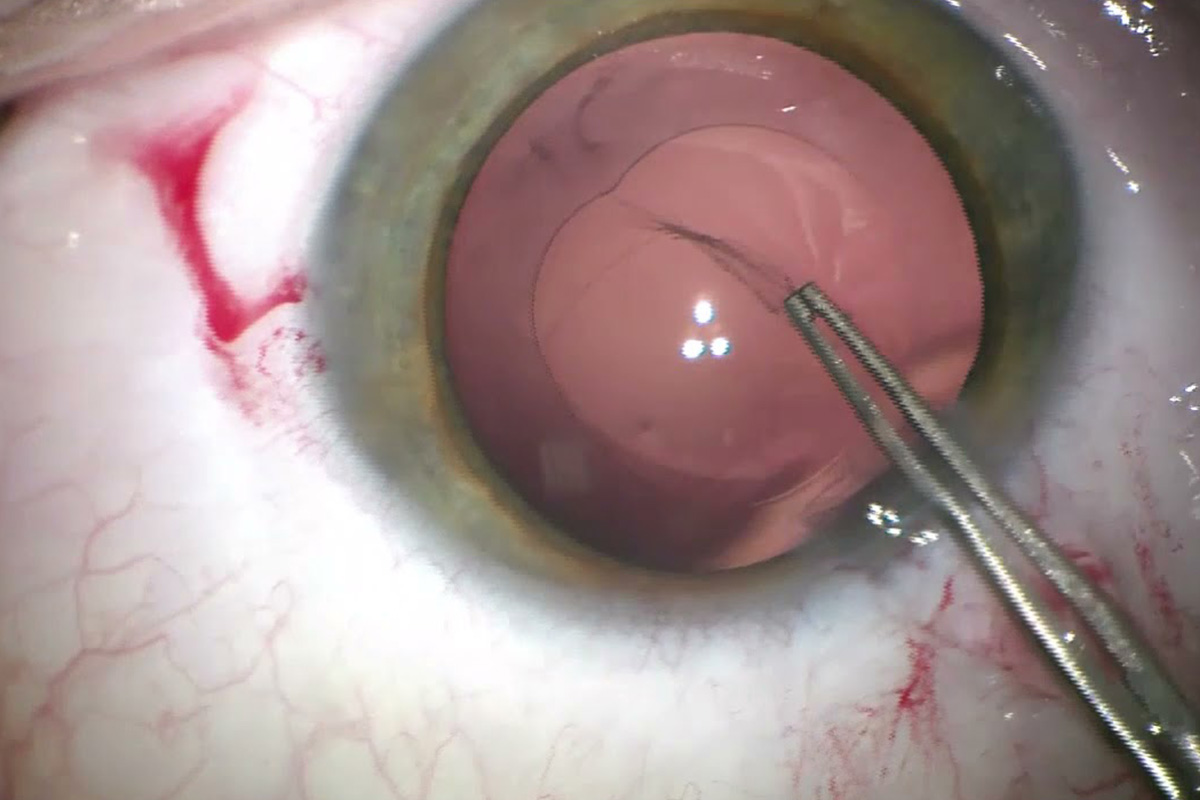
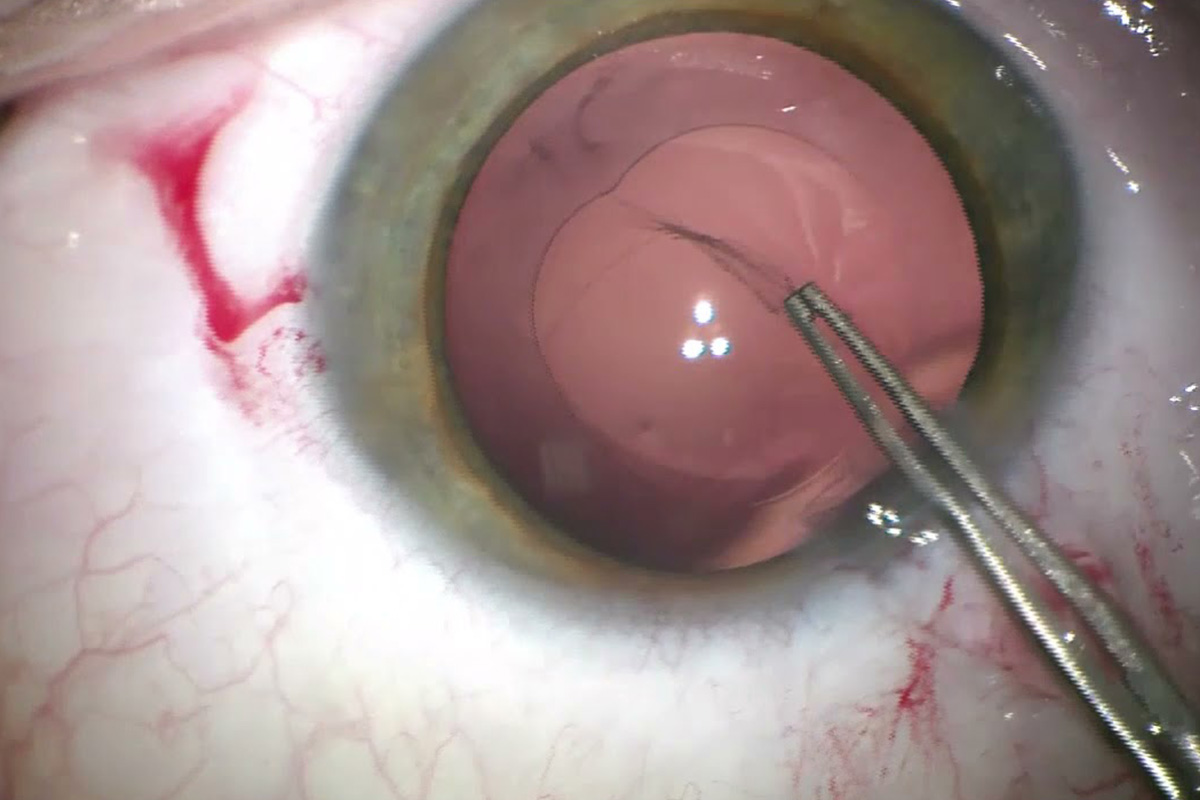
It is possible to remove the entire cataract by aspiration alone because children lack a hard lens nucleus. Congenital cataracts are frequently treated with two procedures.
Lensectomy
The majority of the lens, including the posterior capsule, and the anterior vitreous are removed during a lensectomy. As a result, the visual axis remains perpetually unobstructed. However, it necessitates the use of a vitrectomy machine, and any disruption to the vitreous may raise the possibility of delayed retinal detachment.
I prefer to use an anterior chamber maintainer that is inserted through the cornea. Then, using the vitrector, I extract the anterior lens capsule while keeping the capsule’s edge intact. The vitrector’s cutting action is used to aspirate the lens material and then remove the posterior capsule and anterior vitreous.
An IOL can be inserted at the time of surgery or later as a secondary procedure if the capsule’s rim is still intact.
Extracapsular cataract extraction (ECCE)
A child’s anterior capsule is significantly more flexible than an adult lens. Continuous curvilinear capsulorhexis (CCC) becomes harder as a result. Since the lens material may be easily aspirated with a Simcoe cannula and there is no significant nucleus to extract, the rhexis should be kept little (4–5mm). A regular can opener may also be used to perform a capsulotomy.
The capsule will become opaque if it is not broken. The majority of adult patients do not have posterior capsule opacification that is visually significant. But sooner or later, every child’s eye will require a capsulotomy. At the conclusion of the ECCE, several surgeons conduct a primary capsulotomy. Nonetheless, this sometimes shuts and needs revision, especially among younger children.
I would rather do a lensctomy on the majority of youngsters under the age of five and an ECCE on the majority of older kids. This is because older children are far less likely to develop amblyopia, which means that vision lost due to capsule opacity may be restored. Capsule opacity can cause irreparable amblyopia in younger children and should be avoided.
Intraocular lenses (IOLs)
After surgery, it is critical to treat aphakia in infants as soon as possible. When the cataract is removed, one possibility is to insert an IOL. Regretfully, it’s not that straightforward. The human lens is more spherical at birth than it is in adults. Its strength is around 30D, which makes up for the smaller axial length of an infant’s eye. By the age of five, this drops to between 20 and 22D. This implies that when a baby is older, an IOL that provides them with normal vision will result in significant myopia. Changes in the corneal power and axial lengthening of the globe add more complexity to the situation. Since these changes occur most quickly during the first few years of a child’s life, it is nearly impossible to determine the proper lens power for any given baby.
Although IOL implantation is now commonplace in older children, it is still a very contentious topic in younger children, especially those under the age of two.
After Surgery
With the exception of eye drops and glasses—if necessary—adults don’t need much postoperative treatment. It should be noted from the start that the procedure is just the first step in a lengthy course of therapy for kids.
Refraction
The primary goal is to cure the aphakia, and this should be done as soon as feasible. Contact lenses are popular in wealthy nations. They have adjustable power and are simple to modify. Nonetheless, their need for strict cleanliness renders them unsuitable in environments with poor water and sanitation. Using glasses or an IOL is an alternative. Even with an IOL, there will be some residual refractive error, and glasses will be needed to achieve the finest possible eyesight. The glasses should be fitted as soon as the youngster can wear them. At least every four months until they are two years old, the refraction needs to be monitored frequently; after the age of five, it should be monitored once a year.
Amblyopia
The majority of youngsters born with cataracts will have amblyopia. Due to the cataract blurring the retinal image, the brain is unable to comprehend the data it receives from the eye, and eyesight does not develop correctly. Restoring image clarity by removing the cataract and correcting the aphakia will still require the brain to learn to see, which will take time. Nystagmus can occur if the eyes have never had clear vision because they will not be able to concentrate properly. In children, nystagmus is not a contra-indication to surgery because it frequently goes away when eyesight is regained.
Often, one eye will perform better than the other, and this will become the favorite eye, causing the other eye to become amblyopic. Regularly monitoring the best corrected vision in each eye is the only method to identify this. It is likely that a child is amblyopic and needs occlusion therapy of the preferred eye if one eye is two or more lines worse than the other and there is no other obvious reason for this discrepancy. The first year of life carries the greatest risk of developing amblyopia, which lessens significantly after the age of five.
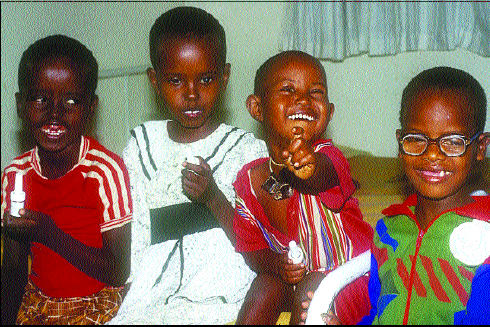
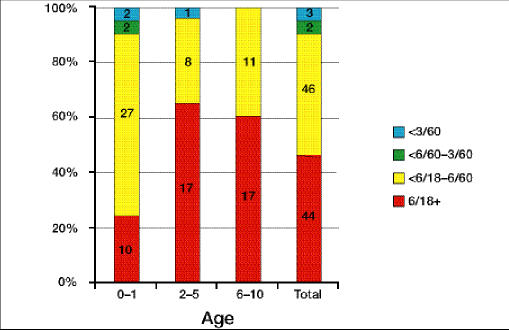
The visual outlook is favorable as long as the best possible treatment is delivered. Only 5% of eyes in Kenya had a visual acuity of less than 6/60, while 47% had a visual acuity of 6/18 or higher. These youngsters will mostly be able to enroll in regular schools.
Complications
Posterior capsule opacification will occur in every child who does not have a posterior capsulotomy. With a needle or a Nd:YAG laser, an aperture can be made in the capsule to treat this. The anterior vitreous and posterior capsule may also be removed using a vitrector. The opacity may return to the anterior hyaloid surface if the capsule is opened without first extracting the vitreous. Regular examinations are the only way to identify the progressive capsule opacity-related loss of vision in one eye, as it will be asymptomatic.
In rare instances, glaucoma can develop following a lensectomy, especially if the procedure is performed during the first week of life. This type of glaucoma is extremely challenging to treat and often causes blindness. Surgery is less likely to restore 6/6 vision if it is postponed until the youngster is three to four months old, but the chance of developing glaucoma is decreased.
Eyes that have undergone surgery for congenital cataracts are more likely to experience retinal detachment. The average time between surgery and its occurrence is 35 years, which is often very late. Even if it occurs years after their procedure for congenital cataract, any patient who reports a sudden loss of vision should be presumed to have retinal detachment unless proven otherwise.
In conclusion
Congenital cataracts are complicated to manage and should only be treated in specialized facilities. Nevertheless, every eye worker may contribute by helping with case identification and follow-up.



