Diabetic foot early signs-various aspects-
Diabetic foot early signs consist of:
- Discomfort: Discomfort, burning sensation, or tingling in the feet
- Dermatological changes: Dry, fissured skin, glossy skin, or thinning hair on the feet
- Inflammation: Enlarged feet or blisters filled with fluid
- Foot contour: A modification in the shape of the feet over time
- Toenail issues: Thick, yellowish toenails
- Foot infections: Athlete’s foot or a foot infection that emits a foul odor and turns black
- Warm areas: A “hot spot” on the foot, which may be an early indication of a blister or ulcer
- Sensory loss: Loss of sensation or the ability to feel heat or cold in the feet
- Corns or callouses: Rough skin patches due to pressure or friction
- Plantar warts: Flesh-colored growths located on the bottom of the feet
Understand All About Early-Stage Diabetic Foot Ulcers!
Individuals with diabetes are 20 times more prone to undergoing amputation.
To avert severe foot complications, you should manage your blood sugar levels and care for your feet daily.


If you have diabetes, you face a higher risk of experiencing foot problems and complications, such as open wounds and infections. Therefore, it’s crucial to take every possible measure to care for your feet to notice-Diabetic foot early signs and effectively manage diabetes. If you encounter foot problems, consult your healthcare provider as soon as you can. Timely treatment is essential to avoid serious complications.
If any patient of ENT requires any surgery, opd consultation or online consultation in clinic of ENT specialist Doctor Dr Sagar Rajkuwar ,he may contact him at the following address-
Prabha ENT clinic, plot no 345,Saigram colony, opposite Indoline furniture Ambad link road, Ambad ,1 km from Pathardi phata Nashik ,422010, Maharashtra, India-Dr Sagar Rajkuwar (MS-ENT), Cell no- 7387590194 , 9892596635
Issued in public interest by –
Overview of Diabetic foot early signs-


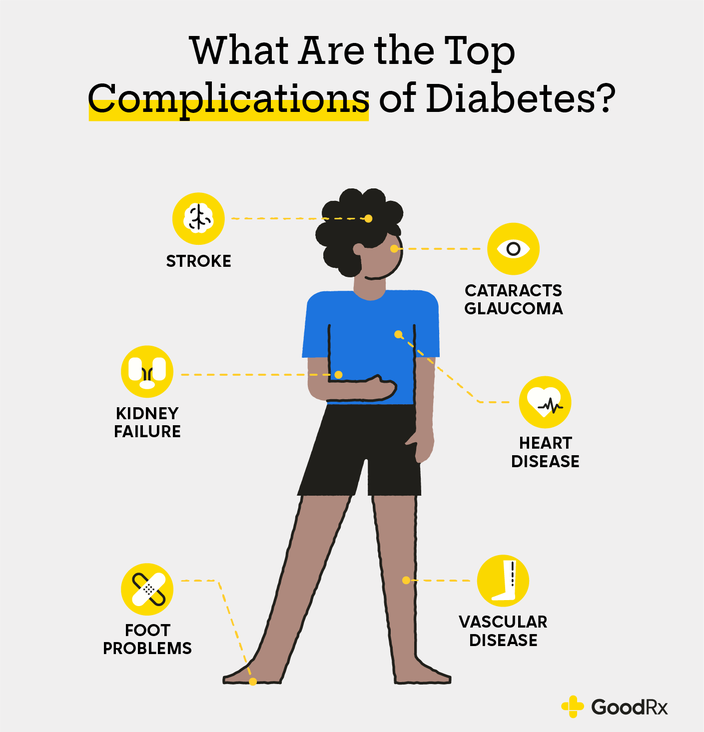
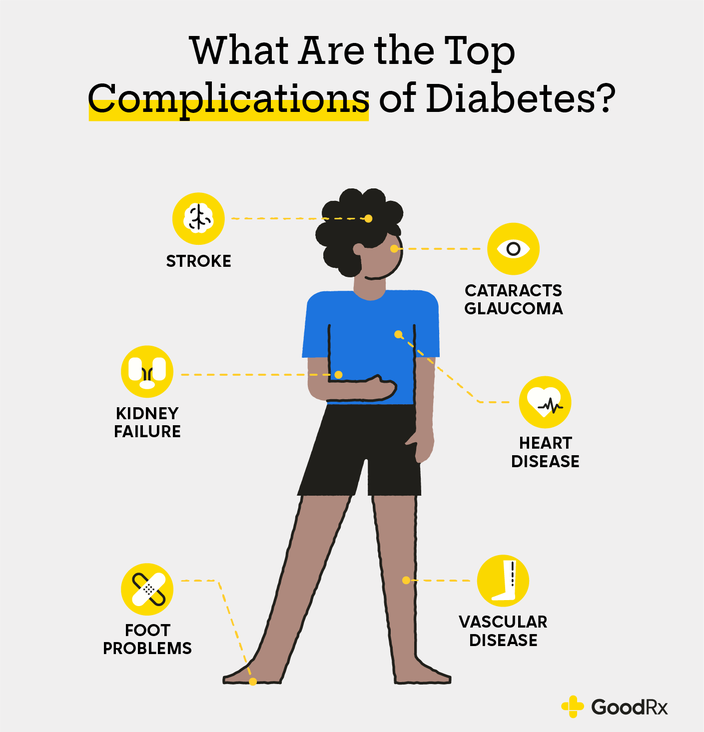
What are conditions related to diabetes affecting the feet?
Individuals with diabetes face a heightened risk of foot conditions and complications if they experience diabetes-related neuropathy and/or poor circulation. Diabetes-related neuropathy occurs when you suffer nerve damage due to consistently elevated blood sugar (hyperglycemia). It predominantly impacts your feet.
Complications associated with diabetes-related foot issues can arise from a chain reaction of problems:
A sore or blister may go unnoticed: Neuropathy induces numbness, tingling, or pain in your feet, making it challenging to realize you have an injury-so it is always better to notice Diabetic foot early signs
The wound can become infected: Individuals with diabetes are at a greater risk of skin infections due to a compromised immune system and inflammation.
The infection may not heal properly: Diabetes can harm blood vessels and diminish blood flow in your feet, which hinders healing.
Slow healing may result in severe complications: If left untreated, infections can spread to other regions of your body and/or result in gangrene (tissue death).
For all these reasons, it is crucial to care for your feet and effectively manage diabetes. A few simple measures can assist you in preventing foot problems.
Types of foot conditions related to diabetes .


Any issue concerning skin, nerves, or circulation in your foot has a heightened likelihood of developing into an infection or another complication when you have diabetes so it is always advisable to notice- Diabetic foot early signs .Instances of foot and toe conditions that might lead to complications include:
- Cuts, ulcers, burns, and blisters that fail to heal.
- Dry, cracked skin.
- Corns and calluses.
- Fungal infections, such as athlete’s foot and toenail fungus.
- Ingrown toenails.
- Hammertoes and bunions.
- Foot ulcers related to diabetes
Foot and toe ulcers (open sores) are some of the most prevalent types of foot issues for individuals with diabetes. Approximately 15% of individuals with diabetes will develop a foot or toe ulcer. These ulcers typically form in areas where your foot consistently rubs or presses against footwear or other surfaces.
Ulcers have the potential to lead to infections. Occasionally, the infection may persist, and it might become necessary to surgically remove part of your foot or toe (amputation). Be aware that early treatment significantly lowers your risk of amputation.
Diabetic foot early signs-


Consult a physician if you experience these symptoms: numbness, ingrown toenail, yellow nails, sores that do not heal, pain or cracked skin.
It is vital to seek medical assistance for foot issues related to diabetes. Avoid attempting to manage them on your own.
What are the symptoms of foot conditions related to diabetes?
The symptoms associated with diabetes-related foot conditions differ depending on the type. However, universally, you should be aware of the following symptoms:
Any alterations to your skin or toenails, including cuts, blisters, calluses, or sores.
- Frequent bleeding.
- Fluid or pus discharge.
- Unpleasant odor.
- Pain.
- Discoloration of the skin.
- Swelling.
Contact your healthcare provider if you notice these Diabetic foot early signs.
What are the complications associated with foot conditions related to diabetes? with respect to-Diabetic foot early signs
The things mentioned below are not Diabetic foot early signs ,but are things found in advanced stages .
Gangrene and Charcot foot are the primary serious complications linked to diabetes-related foot conditions.
Gangrene
An untreated foot infection may lead to gangrene. Gangrene constitutes a medical emergency where blood flow to a particular area of your body ceases, resulting in tissue death in that region. If not treated promptly, gangrene can be life-threatening.
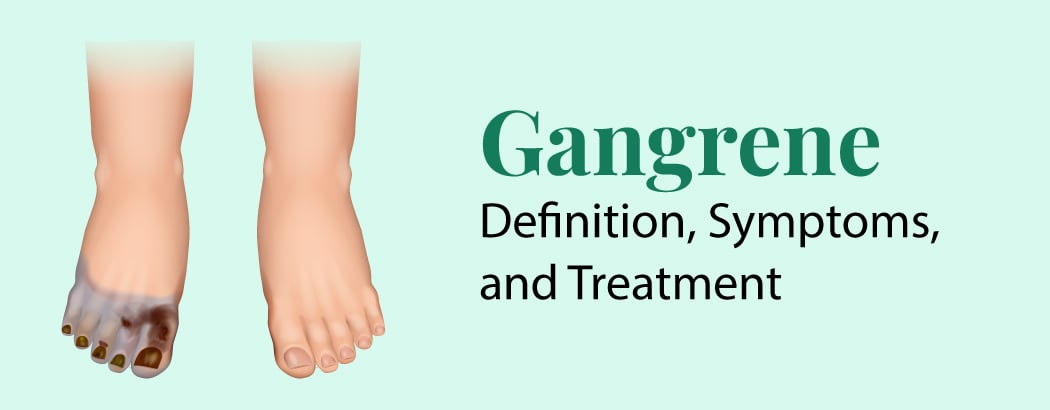
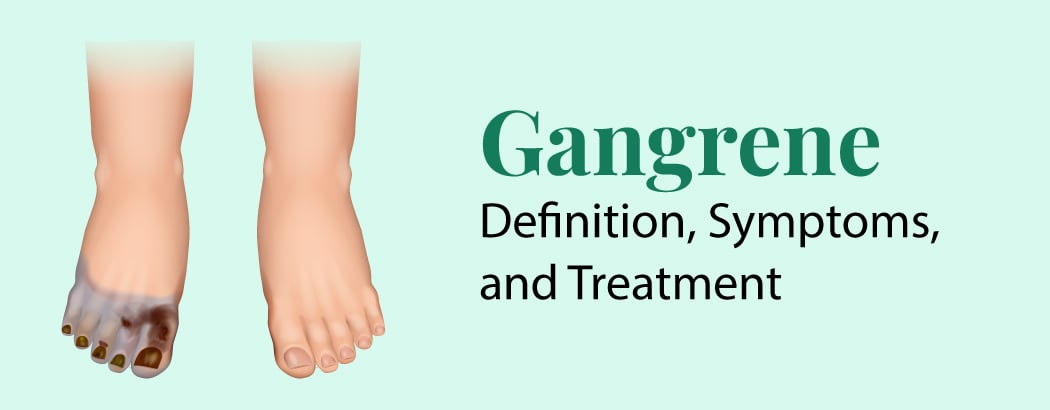
Symptoms of gangrene entail:
- Changes in skin color (shifting from red to brown, eventually turning to purple or greenish-black).
- Swollen skin.
- Intense pain or a sensation of numbness.
- Skin that feels cool when touched.
- A crackling noise upon applying pressure to the skin.
- Sores and blisters that expel blood or emit a foul-smelling discharge.
- Chills.
- Rapid breathing and heart rate.
- Fever.
- Reduced appetite.
- Nausea.
Visit the emergency room (ER) if you notice signs of gangrene.
Charcot foot
Charcot foot is an uncommon complication stemming from diabetes-related neuropathy. If not addressed swiftly, Charcot foot can cause the joints in your foot to collapse, permanently impacting your ability to utilize your foot. It may also increase the risk of a foot infection worsening or spreading throughout your body.
Initial symptoms of Charcot foot consist of:
- Foot pain.
- Discoloration or reddening.
- Swelling.
- A sensation of heat or warmth (especially if one foot feels significantly warmer than the other).
Contact your healthcare provider if you identify these early signs.
What leads to diabetes related foot conditions? in relation to-Diabetic foot early signs
The two primary root causes of foot problems related to diabetes are:
Diabetes-related neuropathy: Neuropathy refers to nerve damage. Diabetes-related neuropathy — specifically peripheral neuropathy — makes it challenging to feel problems with your feet. This can result in a delay in the diagnosis and treatment of foot issues.
Peripheral artery disease (PAD): Individuals with diabetes are at a higher risk of developing PAD, which can impact blood circulation to your legs and feet. Diminished blood flow (poor circulation) can hinder the healing of foot problems (such as sores).
Consistently elevated blood sugar levels can harm nerves and small blood vessels. Since every individual is unique, it is impossible to forecast the exact levels of elevated blood sugar — and the duration needed — to cause neuropathy or PAD. One study involving individuals with Type 2 diabetes indicates that having an A1C exceeding 7% for at least 3 years heightens your risk of diabetes-related neuropathy.
Inadequate foot care, such as using poorly fitting shoes, walking without footwear, or neglecting to treat wounds and cuts ( Diabetic foot early signs )with basic first aid, can also elevate your risk of foot problems.
Diagnosis and Tests in Diabetic foot early signs


How are foot problems related to diabetes diagnosed?
To diagnose diabetes-related foot problems, a healthcare provider will:
- Inquire about your symptoms.
- Ask about your history of diabetes and its management.
- Inspect your toes, feet, and legs.
- Use various tools to touch your toes, feet, and legs to check for numbness.
If you have a diabetes-related ulcer or blister, your provider will likely:
- Inspect it for any signs of infection, such as swelling, warmth, discoloration, or discharge in relation to Diabetic foot early signs
- Suggest imaging tests (like an X-ray or MRI) to identify any deeper issues beneath the skin.
- Collect a sample of the affected skin or drainage (biopsy) to test for infection.
For update on further important health related topics and frequently asked questions on health topics by general population please click on the link given below to join our WhatsApp group –
https://chat.whatsapp.com/Lv3NbcguOBS5ow6X9DpMMA
Issued in public interest by –
Management and Treatment of Diabetic foot early signs


What treatments are available for diabetes-related foot conditions?
The treatment for foot problems associated with diabetes varies based on the specific type. It is crucial to seek medical assistance for diabetes-related foot conditions — refrain from attempting to treat them on your own. Treatment for these concerns may involve a podiatrist — a healthcare professional specializing in foot care.
If you have a diabetes-related ulcer, for instance, your provider may:
- Clean the wound.
- Drain any fluid or pus from the ulcer.
- Remove or excise dead or infected tissue (debridement).
- Apply specialized bandages and ointments to absorb excess fluid, protect the wound, and facilitate healing.
- Prescribe a wheelchair or crutches to alleviate weight on the affected foot (known as offloading).
- Prescribe oral or IV antibiotics to manage and eradicate infection.
Depending on the severity of the infection, your provider may suggest hospitalization. In some cases, amputation might be necessary to prevent the infection from spreading to other areas of your body. Prompt treatment significantly reduces the risk of amputation.
Prevention of Diabetic foot early signs


How can I avert foot problems related to diabetes?
There are multiple measures you can take to assist in preventing diabetes-related foot conditions.
The most crucial step is to effectively manage your blood sugar and diabetes to attempt to prevent or postpone neuropathy and blood flow complications related to diabetes. Regularly visit your diabetes healthcare provider (such as an endocrinologist) for assistance with your management plan so as to detect in time- Diabetic foot early signs.
Your medication requirements will evolve as your life does. Additionally, inquire about advancements in diabetes management technologies, such as continuous glucose monitoring (CGM), that may aid you.
You can also lower the likelihood of foot complications related to diabetes ( Diabetic foot early signs )by:
Checking your feet daily: Look for any alterations and don’t forget to check between your toes. Use a mirror to inspect the bottoms of your feet or seek assistance from someone in case of Diabetic foot early signs.
Keeping your toenails trimmed and filed: Cut your nails straight across using clippers to avoid ingrown toenails, and gently smooth out any sharp edges with a nail file. If you’re unable to see or reach your feet, or if you have thick, yellow nails, have your podiatrist trim your nails.
Wearing socks and shoes that fit correctly: Ensure your socks are not excessively tight and that your shoes fit properly. Some individuals with diabetes opt for therapeutic shoes or shoe inserts (orthotics) to help avert wounds or sores. Before wearing them, confirm that no stones or other objects are in your shoes.
Protecting your feet from extreme temperatures: For instance, when wearing sandals, apply sunscreen on the tops of your feet to prevent sunburn. Keep your feet away from heaters and open flames to prevent burns. In colder weather, wear socks and insulated shoes to keep your feet warm in case if you have noticed -Diabetic foot early signs
Maintaining proper blood flow to your feet: For example, elevate your feet while seated, and frequently wiggle your toes. Remain active, but select activities that are gentler on your feet, such as walking or swimming.
Washing and moisturizing your feet daily: Use warm — not hot — water. Dry them completely afterward, including the spaces between your toes. Then, apply lotion to the tops and bottoms of your feet, avoiding the area between your toes.
Asking your healthcare provider to inspect your feet at each visit in case if you suspect- Diabetic foot early signs- Request that your provider visually examine your feet. At least once annually, undergo a comprehensive foot evaluation (known as a diabetes foot exam), which includes assessing the sensation and blood flow in your feet.
Equally important is to avoid certain actions. Don’t:
Remove calluses or corns on your own if Diabetic foot early signs are detected in patient- Avoid cutting off calluses or corns or using over-the-counter (OTC) products (like patches and liquids) for their removal. Instead, consult your podiatrist regarding the optimal method for managing these conditions.
Smoke: Smoking may harm blood vessels and diminish blood circulation to your feet. If you smoke, seek support to quit.
Soak your feet: This could result in your skin becoming overly dry afterward.
Walk barefoot: Always wear socks, shoes, or slippers — even indoors — to safeguard against foot injuries.
Outlook / Prognosis in case of Diabetic foot early signs
What can I anticipate if I have a foot condition related to diabetes?
Foot conditions associated with diabetes are quite frequent among individuals who have experienced diabetes for an extended period. Despite regular foot examinations and diligent blood glucose control, some individuals with diabetes may still develop infections.
Your outlook regarding-Diabetic foot early signs is influenced by factors such as:
- How promptly you identify the foot issue and receive assistance for it.
- Whether there is an infection and its extent of spread.
- The success of the treatment.
Your healthcare provider will provide you with a clearer understanding of what to expect based on your specific circumstances.
Living With Diabetic foot early signs
When should I consult my healthcare provider regarding foot conditions related to diabetes?
Consult your healthcare provider or foot specialist (podiatrist) if you experience any of these Diabetic foot early signs
- Tingling, burning, or discomfort.
- A sore (such as a blister or ulcer) that does not heal.
- Dry, cracked skin.
- Loss of sensation or ability to feel heat or cold.
- A shift in color and temperature.
- Any alterations in foot shape.
- Thick, yellow toenails.
- A fungal infection, such as athlete’s foot, in between your toes.
- Loss of hair on your toes, feet, and lower legs.
- An ingrown toenail.
Woman early signs of diabetic feet
Changes in toenails, numbness, tingling, pain, alterations in skin color or temperature, and dry or cracked skin are some of the early signs of diabetic feet in women. If a woman experiences any of these symptoms, it is imperative that she consult a healthcare professional for diagnosis and treatment.


The initial indications are shown here in greater detail:
Numbness and tingling:
Diabetes can harm nerves, resulting in numbness or tingling in the feet.
Discomfort:
For some women, especially while engaging in physical activity, foot discomfort may occur.
Variations in the skin:
The skin of diabetic feet may become dry and cracked, or the color may change, becoming red or darker.
Changes in toenails:
Diabetes-related circulatory issues may be indicated by fungal infections or yellow, thick toenails.
foot ulcers:
Open sores known as diabetic foot ulcers can form on the foot, frequently going unnoticed due to nerve injury.
Swelling:
Additionally, swelling in the ankles or feet might be a sign, but it’s important to keep in mind that there could be other reasons for the swelling.
Foot shape changes:
Diabetes can cause alterations to the form of the foot over time, such as bunions or claw toes.
FOR INFORMATION ON DIABETES MELLITUS IN GREAT DETAIL PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION .
For signs of diabetic nerve pain in toes pl click on the link given below–It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION .
FOR INFORMATION IN GREAT DETAIL ON Early signs of diabetic coma PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Early signs of diabetic retinopathy PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Diabetic foot early signs PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Symptoms Of Diabetic Nerve Pain In Toes PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Diabetic neuropathy PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Diabetic diet-Part-2 PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Diabetic diet-Part 3 PL CLICK ON THE LINK GIVEN BELOW-It Is Always Better To View Links From Laptop/Desktop Rather Than Mobile Phone As They May Not Be Seen From Mobile Phone. ,In Case Of Technical Difficulties You Need To Copy Paste This Link In Google Search. In Case If You Are Viewing This Blog From Mobile Phone You Need To Click On The Three Dots On The Right Upper Corner Of Your Mobile Screen And ENABLE DESKTOP VERSION.
If Any Patient of ENT Requires Any Surgery, Opd Consultation Or Online Consultation In Clinic of ENT Specialist Doctor Dr. Sagar Rajkuwar ,He May Contact Him At The Following Address-
Prabha ENT Clinic, Plot no 345,Saigram Colony, Opposite Indoline Furniture Ambad Link Road ,Ambad ,1 km From Pathardi Phata Nashik ,422010 ,Maharashtra, India-Dr. Sagar Rajkuwar (MS-ENT), Cell No- 7387590194, 9892596635
Issued in public interest by –
www.entspecialistinnashik.com



