Knee osteoarthritis-various-aspects-
What is knee osteoarthritis?
When the cartilage in your knee joint breaks down and causes the bones to rub against one another, you have knee osteoarthritis. This friction results in pain and edema in your knee, which causes stiffness. Osteoarthritis is a degenerative joint disease that develops over time as a result of wear and tear. It is quite frequent, and one of the most prevalent joints impacted is the knee, which endures a lot of strain throughout one’s life.
Osteoarthritis in your knee is a chronic, progressive illness for which there is no treatment. Lifestyle adjustments and several therapies are available to alleviate your symptoms and slow its course. However, it usually gets worse over time, and it can eventually result in impairment. As your arthritis worsens, your healthcare professional will keep an eye on it. Surgery is an option when it begins to have a significant impact on your daily life.


The progression of knee osteoarthritis
Osteoarthritis is a progressive illness with a predictable course, although it lacks defined phases in the knee. (Unlike other forms of arthritis in the knee.) Your healthcare provider may describe the severity of your illness using stages or levels. Knowing the course of osteoarthritis can help you comprehend your symptoms and predict what will happen next.
The stages are:
Stage 1 (Minor). The cartilage in your knee joint has some wear and tear at stage 1. You might not have felt any discomfort just yet.
Mild is the second step, at which you may begin to experience pain and stiffness in your knee joint, but there is still sufficient cartilage to prevent the bones from rubbing together.
Stage 3 (Moderate). When you are in the moderate stage, your cartilage has decreased noticeably. This results in greater discomfort, especially when bending, kneeling, walking, and running. After extended periods of inactivity, you may also experience increased stiffness or trouble moving your joint.
Severe knee osteoarthritis, or stage 4, is characterized by near total cartilage loss in the knee, which causes the bones to rub against one another during movement. Your knee is rigid, painful, and maybe immovable. You may want to think about getting a knee joint replacement at this point.
Symptoms and Causes
Osteoarthritis of the knee symptoms
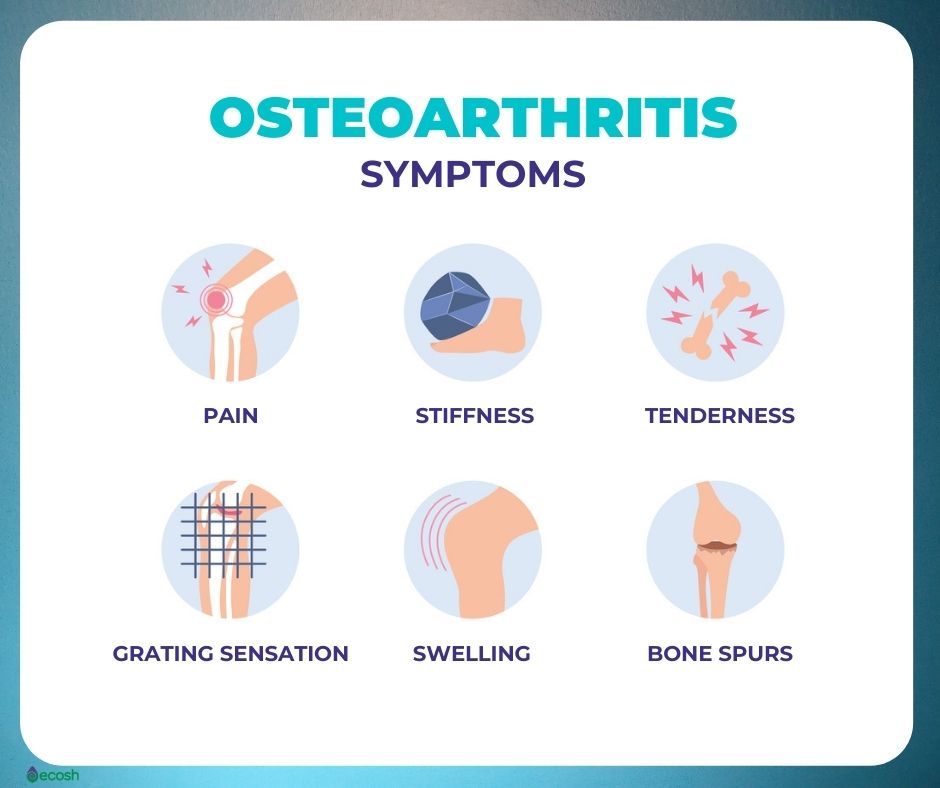
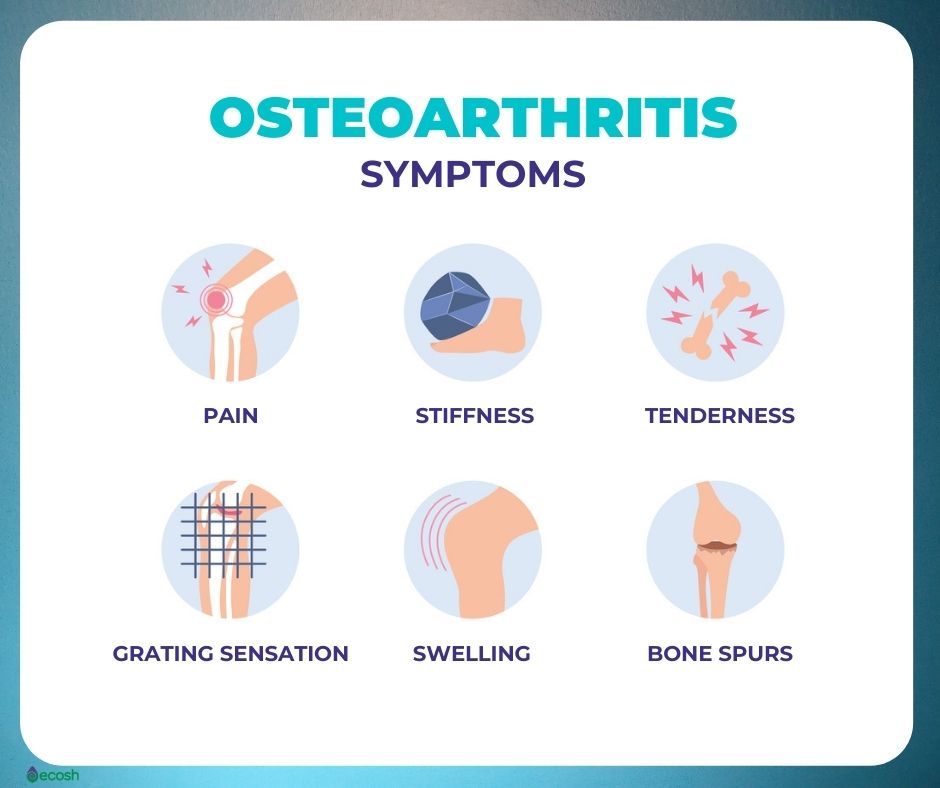
The most typical symptom of knee osteoarthritis is knee pain. When you apply pressure to your knee, move it, or even when you are sitting still, you may experience pain. Additional signs of OA knee include:
- After sitting for a while or when you first stand up, your knee feels stiff.
- Your knee feels puffy or swollen.
- When you move your knee, you hear a crunching or grinding sound.
- Your knee feels unsteady, as though it might give way or buckle.
- When you try to move your knee, it may lock up or feel like it’s stuck.
Potential knee osteoarthritis complications
There are a number of additional adverse effects of knee arthritis as it progresses, such as:
- Joint instability. The muscles that support your knees can weaken as you use them less, which makes the joint less stable. Your walking and risk of harm may be impacted by this.
- Bone spurs. Bone spurs, which are bony protuberances, might develop on your bones as a result of friction and cartilage loss in your joint. These might make your joint more prone to friction and irritation.
- Cyst of Baker. A cyst develops at the back of your knee joint when the synovial membrane that covers your joint capsule protrudes through a tear in the capsule and captures joint fluid in the bulge.
- mood problems. Having OA might increase your risk of experiencing anxiety and depression. New restrictions, mobility difficulties, and persistent pain can all play a role. These might get worse if your attitude is bad.
The cause of knee osteoarthritis is
When the cartilage in your knee joint wears down, you have osteoarthritis of the knee. The ends of your bones are covered with cartilage where they meet in your knee joint. It cushions the bones, enabling them to move freely against one another. When you apply pressure to your knee, it also absorbs shock. The cartilage cannot regenerate if it breaks down. You begin to lose joint movement as you lose it.
In most cases, OA is simply the consequence of the slow deterioration of your joint over time. Other times, minor things, such an injury or excessive strain on the knees, might cause them to wear down more quickly. Similar to the shock absorber in your car, the cartilage in your knees shields it from jolts and bumps. Your shocks will wear out more quickly if you drive on bad roads. Your shocks will last longer if you drive on smooth roads.


The risk factors for knee osteoarthritis
Your knee may be more prone to OA if:
- Your body mass index (BMI) is 30 or higher, which is considered overweight.
- You have a previous knee injury or you hurt your knee.
- At work or when participating in sports, you frequently put pressure on your knee.
- You inherited a propensity to develop osteoarthritis of the knee
- Having “knock knees” or other misaligned bones or joints.
Tests and Diagnosis
What methods do physicians use to determine if a knee has osteoarthritis?
Your doctor will begin by inquiring about your symptoms and doing a physical examination of your knee. They’ll check:
- If your knee is painful, swollen, or discolored
- If you experience discomfort in a particular spot on your knee
- If there are any indicators that you might have hurt your knee
- The degree to which you may move your knee (range of motion)
- if your knee joint feels “loose” or unstable
- The way you move on your knee
They will next conduct imaging exams. An x-ray of the knee will usually reveal evidence of knee osteoarthritis. They may request an MRI or CT scan in some cases if they need a closer examination of the tissues in your joint.
Management and Treatment


What are the treatments for osteoarthritis of the knee?
Lifestyle adjustments, nonsurgical therapies, and surgery are all available treatments for knee osteoarthritis. In general, healthcare professionals will attempt nonsurgical therapies before suggesting surgery for knee OA.
Non-surgical methods of treating knee OA
Non-surgical therapies for knee osteoarthritis include:
- Taking painkillers
- Engaging in physical therapy
- Sometimes losing weight
- With a knee brace
- Injections of cortisone (a steroid)
- Viscosupplementation via knee gel injections
- Injections of a genicular nerve block
- Injections of platelet-rich plasma
Surgical procedures for knee OA
Among the surgical methods for treating knee osteoarthritis are the following:
- Changing the cartilage
- Reshaping the knee bone (osteotomy)
- Partial knee replacement
- Complete knee replacement
Prevention
Is it possible to avoid knee osteoarthritis?
You can’t completely avoid knee osteoarthritis because it typically has multiple causes. However, you may lessen your risk by minimizing stress and strain on your knee joint whenever possible. For instance:
- Think about ways to alter how you perform your job if it puts stress on your knees.
- Choose softer surfaces over pavement if you run or jog.
- Mix up your workout schedule with low-impact activities such swimming or cycling.
- Losing only 10% of your excess weight can greatly lower your chances of developing knee OA.





