Osteoarthritis causes-various-aspects-
The breakdown of cartilage within joints, which results in pain, stiffness, and limited range of motion, is the main cause of osteoarthritis. The onset of osteoarthritis is influenced by a variety of variables, such as age, weight, joint injuries, and heredity.
Summary
Millions of people around the world suffer from osteoarthritis, which is the most prevalent kind of arthritis. This occurs when the protective cartilage that cushions the ends of the bones breaks down over time.
Osteoarthritis can harm any joint, but it most frequently targets the spine, hips, knees, and hands.
Although the injury to joints cannot be repaired, the symptoms of osteoarthritis can typically be controlled. Receiving specific therapies, keeping active, and maintaining a healthy weight can all help to slow the course of the illness and enhance joint function and pain.


Symptoms
The symptoms of osteoarthritis often appear gradually and worsen with time. Osteoarthritis symptoms include:
- Pain. The afflicted joints may be painful both during and after movement.
- Rigidity. Stiffness of the joints can be most apparent after being inactive or upon waking up.
- Tenderness. You may experience tenderness in your joints when you apply moderate pressure to or around them.
- Lack of versatility. It may be difficult for you to move your joint through its whole range of motion.
- feeling of gritting one’s teeth. The joint may produce a grating feeling, and you may hear popping or crackling noises.
- Osteophytes. Additional pieces of bone that feel like hard knots might grow surrounding the afflicted joint.
- Swelling. Inflammation of the soft tissue surrounding the joint may be the reason for this.
Causes
When the cartilage that cushions the ends of bones in the joints slowly wears away, osteoarthritis develops. Cartilage is a strong, slick tissue that enables practically friction-free joint movement.
Eventually, bone will rub on bone if the cartilage wears away entirely.
The cartilage is not the only thing impacted by osteoarthritis. Additionally, it has an impact on the whole joint. It weakens the powerful bands of tissue that link the joint together and connects muscle to bone, as well as causing modifications to the bone. Additionally, it could result in swelling of the joint lining.
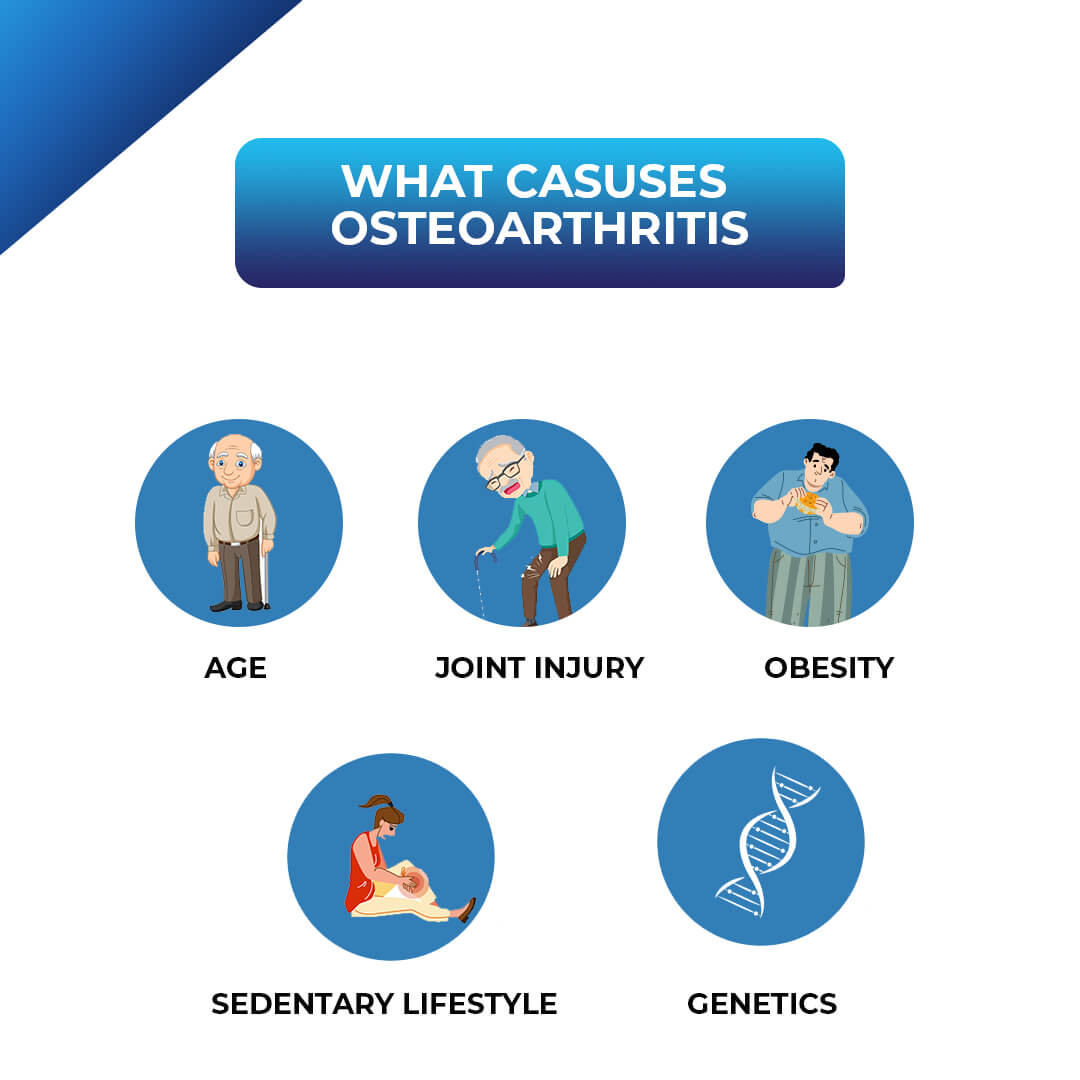
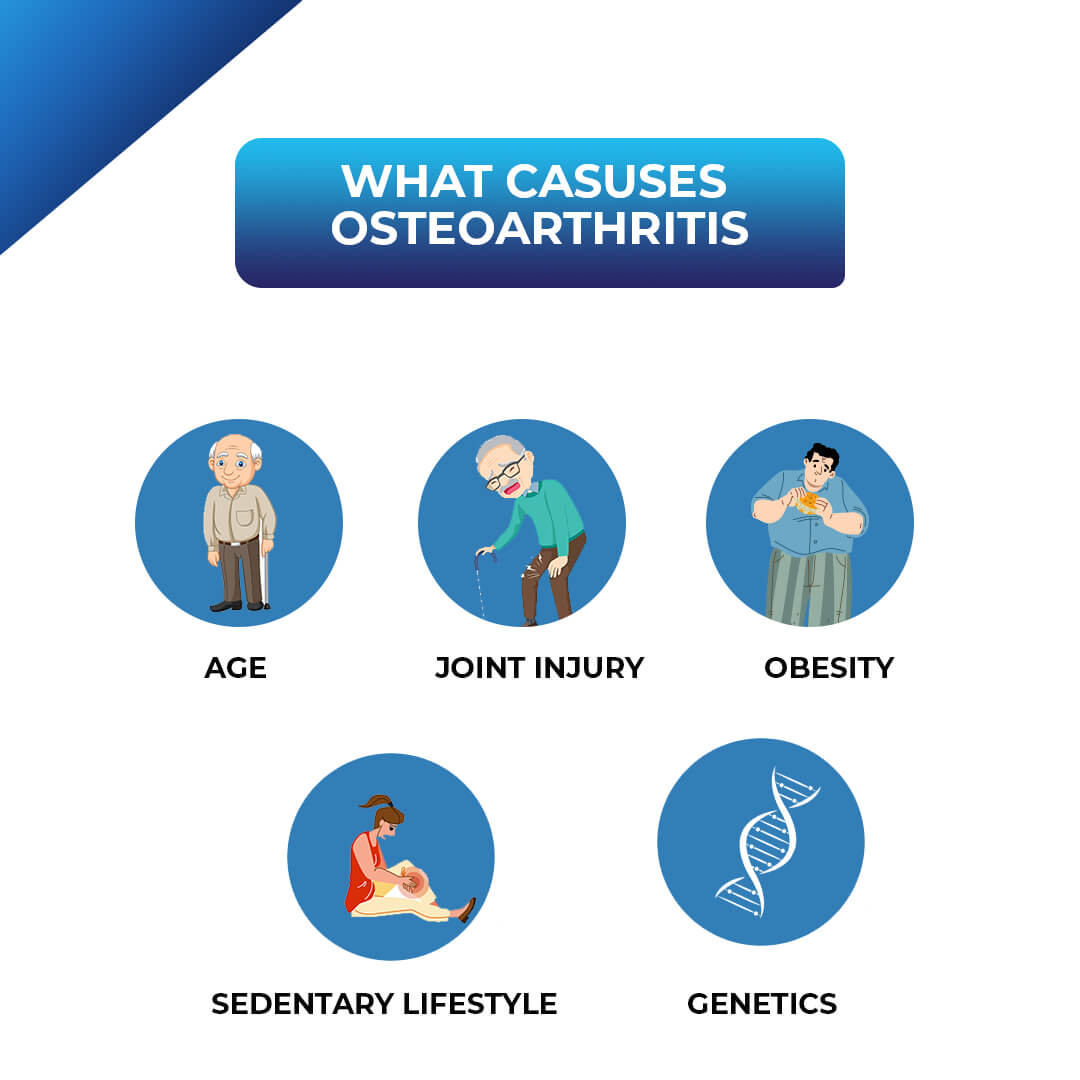
The major causes of osteoarthritis are listed here:
1. Age and Wear & Tear:
Age:
The prevalence of OA rises with age. The cartilage becomes more vulnerable to injury as we age since it gradually wears out over time.
Wear and Tear:
In weight-bearing joints like the knees and hips, cartilage may deteriorate due to frequent use and stress on the joints.
2. Abuse and Injury:
Joint Injuries:
The likelihood of developing OA in the afflicted joint might be increased by prior injuries like ligament tears, dislocations, or fractures.
Overuse:
Cartilage can be harmed by repetitive actions or motions that place too much pressure on a joint.
3. Body Structure and Genetics:
Genetics: Certain people may be genetically predisposed to acquiring OA.
Bone Abnormalities: The likelihood of developing OA may be raised by abnormal joint development or bone deformities.
4. Obesity:
Weight: Carrying extra weight increases the strain on weight-bearing joints such the knees and hips, which can hasten the deterioration of cartilage.
5. Other Considerations:
Gender:
OA is more common among women than men.
Metabolic disorders:
The likelihood of developing OA can be raised by conditions like diabetes and some metabolic diseases that lead to cartilage degradation.
Inactive Lifestyle:
A lack of exercise might weaken the muscles that support joints, increasing their risk of injury and OA.
Changes in Hormones:
A decrease in estrogen levels following menopause may also contribute to cartilage deterioration.
Some Occupations:
The risk of osteoarthritis can be increased by jobs that require repeated motions or extended periods of kneeling, squatting, or lifting.
Osteoarthritis causes in young adults
Several factors, such as injuries, excessive usage, inherited predispositions, obesity, and lifestyle decisions like smoking, can cause osteoarthritis to manifest in young adults. Fractures and dislocations are examples of joint injuries that can impair the joint’s normal structure and raise the likelihood of developing osteoarthritis later in life. Osteoarthritis and cartilage injury can also result from overuse, particularly in strenuous occupations or sports. Due to the increased pressure that obesity places on weight-bearing joints like the knees and hips, cartilage degradation is accelerated. Genetics also contribute, with some people inheriting a proclivity for osteoarthritis development.
The reasons are explained in greater detail in the following:
1. Injuries to Joints:
Fractures or Dislocations:
These can harm the joint’s ligaments, bones, and cartilage, increasing its vulnerability to osteoarthritis.
Ligament rupture:
The joint is kept stable by ligaments. Crying might cause joint instability and raise the chance of developing osteoarthritis.
Cartilage Injury:
Cartilage can be directly harmed by injuries, which reduces its capacity to absorb joint stress.
2. Excessive Use and Repetitive Stress:
Games:
Particularly if the technique is bad or the person is overtraining, high-impact activities like football, hockey, and running might place a lot of strain on the joints.
Activities Related to One’s Occupation:
Osteoarthritis can also be brought on by jobs that need a lot of lifting, repetitive motions, or extended periods of sitting.
3. Obesity:
Higher Level of Stress:
Excess weight increases the strain on weight-bearing joints like the knees and hips.
Inflammation:
Inflammation in and around joints can be caused by obesity, which hastens the breakdown of cartilage.
4. Genetics:
Family Background:
Osteoarthritis is more likely to develop if there is a family history of the disease.
Inborn Problems:
People with deformed joints or damaged cartilage are more prone to developing osteoarthritis.
5. Lifestyle-related Variables:
Smoking:
Blood supply to cartilage may be reduced by smoking, which impairs its capacity for self-healing.
Insufficient Sleep:
Insufficient sleep might exacerbate osteoarthritis symptoms and contribute to inflammation.
6. Additional risk variables:
Specific Metabolic Disorders: Osteoarthritis risk can be raised by diseases like diabetes.
Infections: Certain infections, such Lyme disease, can cause joint inflammation, which may result in osteoarthritis.
Autoimmune illnesses such lupus can cause chronic inflammation and joint damage, which raises the risk of osteoarthritis.
Osteoarthritis causes inflammation
Indeed, osteoarthritis is an inflammatory disease that causes inflammation in the joints, especially in the cartilage and bone. Inflammation is a major contributor to the onset and progression of osteoarthritis, even though it is sometimes thought of as a degenerative illness.
Elaboration:
What is osteoarthritis?
Osteoarthritis (OA) is a degenerative disorder in which the cartilage in joints progressively wears away, causing bone-on-bone contact.
The Function of Inflammation:
A major process in OA is inflammation. It entails the release of inflammatory mediators by a variety of cells, including those in the joint and other tissues such adipose tissue. These mediators have the potential to harm the synovial membrane (the lining of the joint capsule), cartilage, and bone.
Inflammation Triggers:
In osteoarthritis, inflammation can be brought on by a variety of factors, including external mediators (cytokines and proteases) and internal cellular processes (increased production of inflammatory mediators, accumulation of oxidized proteins, and advanced glycation endproducts).
Symptoms of Inflammation:
Joint discomfort, edema, stiffness, and occasionally redness are signs of inflammation in osteoarthritis.
How OA develops:
Inflammation may hasten the breakdown of bone and cartilage, resulting in more joint discomfort and harm.
Treatment Priority:
Pain relievers and treatments that aid in lowering inflammation, such nonsteroidal anti-inflammatory drugs (NSAIDs) and physical therapy, are common treatments for OA.
Risk factors
Osteoarthritis risk factors include:
Advancing age. The likelihood of developing osteoarthritis rises with age.
Sex as determined at birth. Although the reason is unknown, those born with female sex are more prone to getting osteoarthritis.
Obesity. Having excessive body weight increases the likelihood of developing osteoarthritis in a number of ways. Your risk increases with your weight. Weight-bearing joints like the hips and knees are
subjected to more stress when a person gains weight. Fat tissue also produces proteins that can lead to detrimental swelling in and around your joints.
Injuries to the joints. Accidents and sports injuries can raise the chance of developing osteoarthritis. The likelihood of developing osteoarthritis might be raised by injuries that happened even years ago.
Constant joint stress. Osteoarthritis can develop in a joint at any point in time if a work or sport causes repeated stress to it.
Genetics. The predisposition to get osteoarthritis can be passed down via heredity.
Deformities of the bones. Some individuals are born with damaged cartilage or deformed joints.
Some metabolic illnesses, such as diabetes and hemochromatosis, which is a condition where your body has an excessive amount of iron.
Problems
Osteoarthritis is a progressive condition that frequently causes persistent discomfort. Joint discomfort and stiffness can become so bad that it is hard to complete daily activities.
Osteoarthritis’s pain, stiffness, and mobility problems can lead to depression and sleep disorders.
Different kinds of osteoarthritis
Osteoarthritis may be classified as one of two categories by a healthcare professional:
- The most prevalent kind of arthritis that develops in your joints over time is primary osteoarthritis. Normal wear and tear from utilizing your joints over the course of your life, according to experts, is the most frequent cause.
- When something directly injures one of your joints enough to result in osteoarthritis, secondary osteoarthritis develops. Secondary osteoarthritis is frequently caused by injuries and trauma. Additionally, other forms of arthritis can inflict sufficient harm to the cartilage in your joints to result in osteoarthritis.
What is the prevalence of osteoarthritis?
Osteoarthritis is quite prevalent. According to experts, over 80% of persons over 55 have osteoarthritis, regardless of whether they ever manifest symptoms.
About 60% of persons with osteoarthritis experience symptoms that they can see or feel.
What are the treatments for osteoarthritis?
With the help of your healthcare practitioner, you may discover therapies that ease the symptoms of your osteoarthritis. Unfortunately, there is no cure for arthritis, and you cannot regenerate the cartilage in your afflicted joints. When you have symptoms, your provider will assist you in figuring out how to handle them.
The most prevalent therapies for osteoarthritis are:
- Treatment: OTC pain relievers can help alleviate discomfort and inflammation. You may require topical pain relievers (creams, ointments, or patches that you apply to your skin close to the afflicted joints) or medicine that you take orally.
- Physical activity can help ease stiffness and strengthen the muscles surrounding your joints. Weight training, water aerobics, swimming, and other low-impact activities can all be beneficial. Your provider may suggest that you collaborate with a physical therapist.
- Supportive aids: You can support and stabilize your joints by wearing shoe inserts or a brace. Using a cane or walker can relieve strain on your injured joints and aid in safe movement.
- Therapies for heat and cold: Applying heat or cold to your affected joints may help alleviate stiffness and discomfort. Your provider will advise you on the frequency and duration of using a heating pad, ice packs, or cool compress.
- Low-dose radiation therapy (LDRT): This therapy employs low doses of radiation to help alleviate joint inflammation. It might be an option for those with early-stage osteoarthritis who are looking to avoid surgery or drugs.
- Complementary treatment: This type of therapy may be used in conjunction with other course of therapy. Massage, meditation, tai chi, dietary supplements, and acupuncture are a few examples of complementary medicine. Before beginning any herbal or dietary supplements, speak with your healthcare provider.
- Surgery: The majority of those with osteoarthritis do not require surgical intervention. If you are experiencing severe symptoms and other therapies have failed, your provider may suggest surgery. A joint replacement (arthroplasty) may be necessary. Your doctor or surgeon will explain what to anticipate.
What steps can I take to make living with osteoarthritis less stressful?
You may need to adjust your schedule to make life with osteoarthritis simpler. Depending on the timing and severity of your symptoms, you might need to change a few things. When managing symptoms, you may need to change or avoid some of your activities. If you require assistance with any of your activities, you may consult an occupational therapist. everyday duties. Occupational therapists are medical professionals who can help you deal with physical issues like arthritis. They can suggest:
- Adaptive tools, such as jar openers.
- Tips for participating in hobbies, sports, or other activities in a safe manner.
- Recommendations on how to lessen joint discomfort during arthritis flare-ups.
When should I see my healthcare provider?
See a healthcare professional right away if you experience any signs of osteoarthritis. Even slight joint discomfort might be a sign that you need care, particularly if it doesn’t go away after a few days.
Beginning osteoarthritis treatment can halt additional deterioration inside your joints, but you cannot fix any cartilage degeneration (breakdown) that has previously occurred.
If your symptoms seem to be returning more frequently or are worse than before, speak with your doctor. If you feel that your current treatments aren’t as effective as they should be, speak with your healthcare professional about alternative treatment options or adjustments you may make to your existing ones.




