Myocardial Infarction Medications-various aspects-
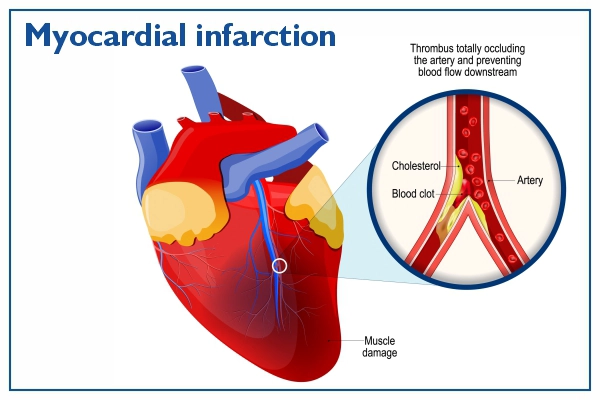
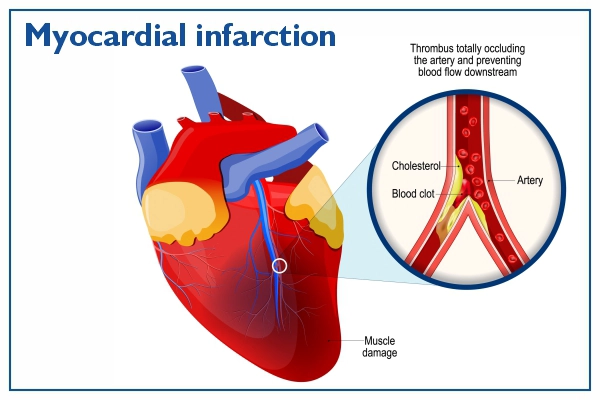
Myocardial infarction (MI) occurs when blood flow to a part of the heart is blocked, usually by a blood clot, leading to damage or death of heart muscle tissue. Prompt medical treatment and pharmacological intervention are essential to restore blood flow, minimize myocardial damage, and prevent complications. The goal of drug therapy in MI is to:


- Re-establish coronary blood flow
- Reduce myocardial oxygen demand
- Prevent further clot formation
- Minimize infarct size
- Prevent complications such as arrhythmias, heart failure, or recurrent infarction
If Any Patient of ENT Requires Any Surgery, Opd Consultation Or Online Consultation In Clinic of ENT Specialist Doctor Dr. Sagar Rajkuwar ,He May Contact Him At The Following Address-
Prabha ENT Clinic, Plot no 345,Saigram Colony, Opposite Indoline Furniture Ambad Link Road ,Ambad ,1 km From Pathardi Phata Nashik ,422010 ,Maharashtra, India-Dr. Sagar Rajkuwar (MS-ENT), Cell No- 7387590194, 9892596635
1. Antiplatelet Agents
These medications reduce platelet aggregation and prevent thrombus formation in coronary arteries.
Aspirin
- Mechanism: Irreversibly inhibits COX-1 and COX-2, reducing thromboxane A2, a promoter of platelet aggregation.
- Use: First-line treatment in acute MI. A loading dose (usually 160–325 mg) is given immediately, followed by a maintenance dose (75–100 mg daily).
- Side effects: GI bleeding, peptic ulcers, hypersensitivity.
P2Y12 Inhibitors (Clopidogrel, Prasugrel, Ticagrelor)
- Mechanism: Inhibit the P2Y12 ADP receptor on platelets, reducing aggregation.
- Use: Combined with aspirin as dual antiplatelet therapy (DAPT) for at least 12 months post-MI.
- Side effects: Bleeding, dyspnea (especially with Ticagrelor), thrombocytopenia.
- Note: Ticagrelor is often preferred due to faster and more potent action.
2. Anticoagulants
Prevent clot extension and new thrombus formation.
Unfractionated Heparin (UFH)
- Mechanism: Binds to antithrombin III, inhibiting thrombin and factor Xa.
- Use: Often used during percutaneous coronary intervention (PCI) or in hospitalized MI patients.
- Side effects: Bleeding, heparin-induced thrombocytopenia (HIT).
Low Molecular Weight Heparin (LMWH) – Enoxaparin
- Use: Alternative to UFH, especially in non-ST-elevation MI (NSTEMI).
- Advantages: Longer half-life, subcutaneous administration.
- Monitoring: Less intensive than UFH.
Bivalirudin
- Use: Anticoagulant during PCI, especially in patients with heparin allergy or HIT risk.
3. Thrombolytics (Fibrinolytics)
Used when PCI is unavailable within the recommended time frame for ST-elevation myocardial infarction (STEMI).
Alteplase (tPA), Reteplase, Tenecteplase
- Mechanism: Activate plasminogen to plasmin, breaking down fibrin clots.
- Use: STEMI within 12 hours of symptom onset, if PCI cannot be performed within 90-120 minutes.
- Contraindications: Active bleeding, history of hemorrhagic stroke, recent surgery.
- Side effects: Intracranial hemorrhage, systemic bleeding.
4. Beta-Blockers
Reduce myocardial oxygen demand by decreasing heart rate, contractility, and blood pressure.
Examples: Metoprolol, Atenolol, Carvedilol
- Use: Initiated within the first 24 hours if no contraindications (e.g., hypotension, bradycardia, heart block).
- Benefits: Reduce infarct size, arrhythmias, and mortality.
- Side effects: Bradycardia, hypotension, bronchospasm (non-selective beta-blockers).
For Update On Further Important Health Related Topics And Frequently Asked Questions On Health Topics By General Population Please Click On The Link Given Below To Join Our WhatsApp Group –
https://chat.whatsapp.com/Lv3NbcguOBS5ow6X9DpMMA
5. Nitrates
Relieve chest pain by vasodilation, reducing preload and myocardial oxygen demand.
Nitroglycerin
- Forms: Sublingual, IV, topical.
- Use: Acute chest pain, hypertension, or heart failure post-MI.
- Side effects: Headache, hypotension, reflex tachycardia.
- Caution: Avoid with PDE-5 inhibitors (e.g., sildenafil).
6. ACE Inhibitors / ARBs
Prevent adverse ventricular remodeling, lower BP, and reduce mortality.
ACE Inhibitors: Lisinopril, Ramipril
ARBs: Losartan, Valsartan (used if ACE inhibitors not tolerated)
- Use: All patients with LVEF <40%, anterior MI, diabetes, or hypertension.
- Side effects: Cough (ACE-I), hyperkalemia, hypotension, angioedema.
7. Statins
Lower LDL cholesterol and stabilize atherosclerotic plaques.
Examples: Atorvastatin, Rosuvastatin (high-intensity)
- Use: Initiated early post-MI regardless of baseline cholesterol.
- Benefits: Reduce future cardiovascular events.
- Side effects: Myopathy, liver enzyme elevation.
- Monitoring: Liver function tests, CK levels if symptomatic.
8. Aldosterone Antagonists
Provide additional mortality benefit in patients with reduced ejection fraction (LVEF <40%) and heart failure or diabetes post-MI.
Examples: Spironolactone, Eplerenone
- Mechanism: Inhibit aldosterone, reduce sodium/water retention, and prevent cardiac remodeling.
- Side effects: Hyperkalemia, gynecomastia (with spironolactone).
DISCLAIMER-Some patients go to net and directly take treatment from there which can lead to catastrophic consequences-Then- Many people ask then why to read all this text -the reason is that it helps you to understand the pathology better ,you can cooperate with treatment better ,your treating physician is already busy with his patients and he does not have sufficient time to explain you all the things right from ABCD ,so it is always better to have some knowledge of the disease /disorder you are suffering from.
9. Pain Control (Analgesics)
Morphine
- Use: For chest pain unrelieved by nitrates.
- Mechanism: Opioid receptor agonist, also causes venodilation.
- Caution: May reduce absorption of antiplatelets (delayed gastric emptying); use judiciously.


10. Glycoprotein IIb/IIIa Inhibitors (in selected PCI cases)
Examples: Abciximab, Eptifibatide
- Mechanism: Block final common pathway for platelet aggregation.
- Use: In high-risk patients undergoing PCI, often with heparin.
- Side effects: Bleeding, thrombocytopenia.
Post-MI Medication Summary (“ABCDEF” Mnemonic)
- A: Aspirin + Antiplatelet (P2Y12) + ACE Inhibitor
- B: Beta-Blocker
- C: Cholesterol control (Statin) + Cessation of smoking
- D: Diet modification + Diabetes management
- E: Exercise + Ejection fraction monitoring
- F: Flu vaccination + Follow-up
Clinical Considerations
- Timing is critical in MI treatment. Antiplatelets and reperfusion strategies (PCI or thrombolysis) must be initiated as early as possible.
- Individualization is important: Patients with renal dysfunction, bleeding risks, or other comorbidities may need dosage adjustments or alternative agents.
- Adherence to long-term medications post-MI is crucial to prevent recurrence and improve survival.
Conclusion
Medication therapy in myocardial infarction is multifaceted, targeting several mechanisms including thrombosis, ischemia, remodeling, and cholesterol management. The choice of drugs depends on the MI type (STEMI vs NSTEMI), patient comorbidities, and timing of presentation. Adherence to evidence-based pharmacological regimens significantly improves long-term outcomes and survival.
FOR INFORMATION IN GREAT DETAIL ON Myocardial Infarction PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Myocardial Infarction Treatment PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Myocardial Infarction Symptoms PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
If any patient has any ENT -Ear nose throat problems and requires any , consultation ,online consultation ,or surgery in clinic of ENT specialist Doctor Dr Sagar Rajkuwar ,he may TAKE APPOINTMENT BY CLICKING ON THE LINK GIVEN BELOW-
Clinic address of ENT SPECIALIST doctor Dr Sagar Rajkuwar-
Prabha ENT clinic, plot no 345,Saigram colony, opposite Indoline furniture Ambad link road ,Ambad ,1 km from Pathardi phata Nashik ,422010 ,Maharashtra, India-Dr Sagar Rajkuwar (MS-ENT), Cel no- 7387590194 , 9892596635



