Cutaneous Rhinosporidiosis-various aspects-
Introduction
Rhinosporidiosis is a chronic granulomatous disease caused by Rhinosporidium seeberi, an aquatic protist that predominantly affects the mucous membranes, especially the nasal and ocular mucosa. While nasal rhinosporidiosis is the most common presentation, cutaneous rhinosporidiosis is a rare but increasingly recognized form. This skin involvement can occur either independently or in association with mucosal lesions. Though rare, cutaneous rhinosporidiosis poses a diagnostic challenge due to its diverse clinical manifestations and resemblance to other chronic dermatoses and infections.
Etiology and Causative Agent
The causative organism, Rhinosporidium seeberi, was historically misclassified as a fungus but is now considered a mesomycetozoan, belonging to the class Mesomycetozoea—a group of protists at the animal-fungal boundary. It thrives in stagnant water bodies like ponds and lakes and is endemic in certain parts of the world, especially South Asia, with high prevalence in India (particularly Tamil Nadu, Kerala, and Odisha), Sri Lanka, and parts of Africa and South America.
Infection typically occurs when traumatized epithelial surfaces are exposed to contaminated water, allowing the organism to invade the host tissue. It does not spread from person to person.
If Any Patient of ENT Requires Any Surgery, Opd Consultation Or Online Consultation In Clinic of ENT Specialist Doctor Dr. Sagar Rajkuwar ,He May Contact Him At The Following Address-
Prabha ENT Clinic, Plot no 345,Saigram Colony, Opposite Indoline Furniture Ambad Link Road ,Ambad ,1 km From Pathardi Phata Nashik ,422010 ,Maharashtra, India-Dr. Sagar Rajkuwar (MS-ENT), Cell No- 7387590194, 9892596635
Pathogenesis
Rhinosporidium seeberi enters the host through abrasions or microtrauma in the skin or mucosa. Once inside, it forms large, thick-walled sporangia within the subepithelial tissue. These sporangia mature and release numerous endospores into the surrounding tissue, causing a chronic granulomatous inflammatory response. The organism can spread by:
- Autoinoculation from mucosal lesions to nearby skin
- Hematogenous dissemination, though rare
- Direct inoculation, leading to primary cutaneous rhinosporidiosis
The presence of mature and immature sporangia at various levels in the tissue leads to a persistent inflammatory response and tissue proliferation.
Clinical Manifestations of Cutaneous Rhinosporidiosis
Cutaneous rhinosporidiosis presents in a variety of forms, making clinical diagnosis challenging. It can occur in three main ways:
1. Satellite Cutaneous Lesions
These occur adjacent to mucosal lesions (e.g., nasal or ocular), due to autoinoculation. The lesions may be small nodules or papules and usually appear around the nose, face, or eyes.
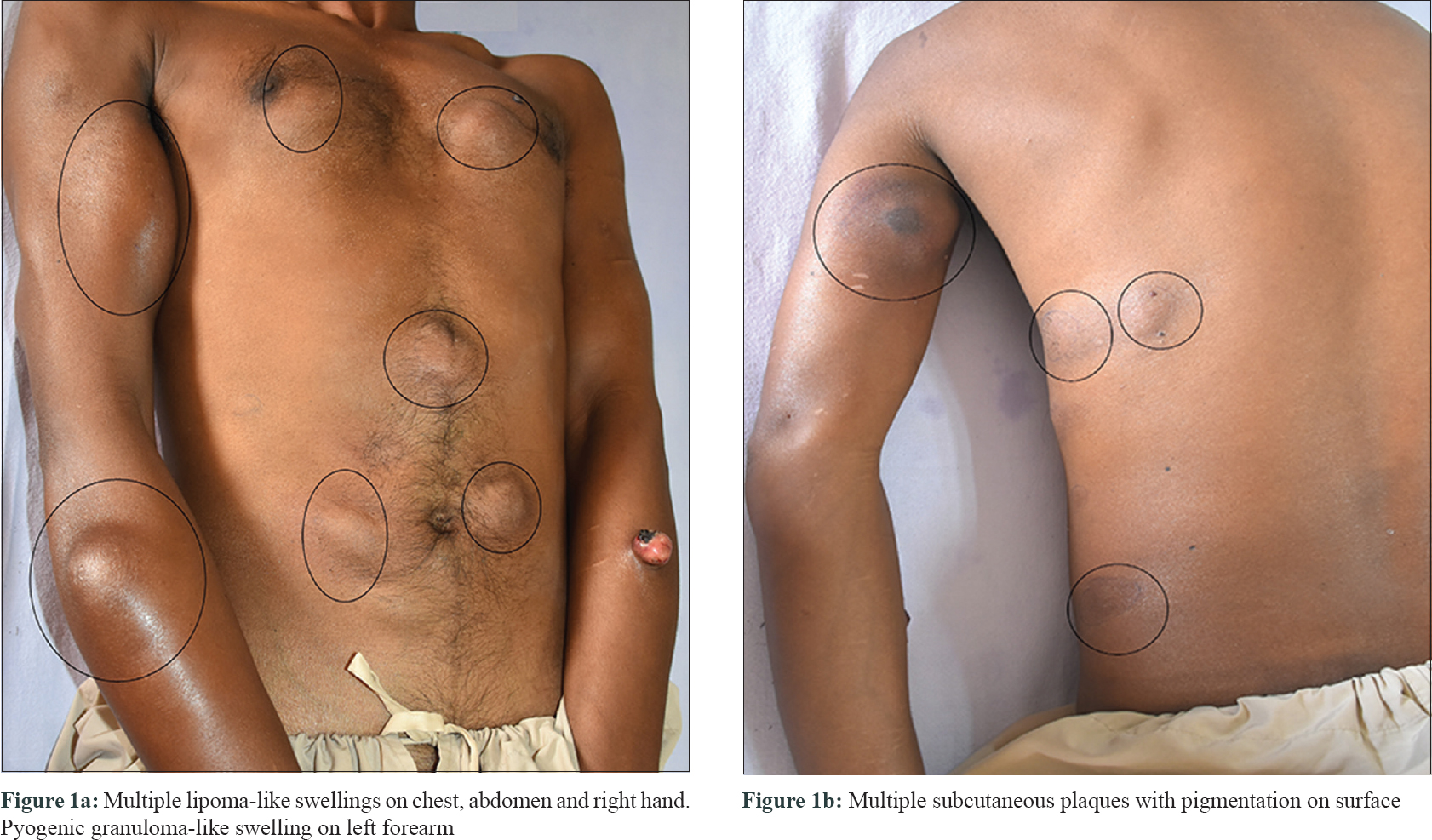
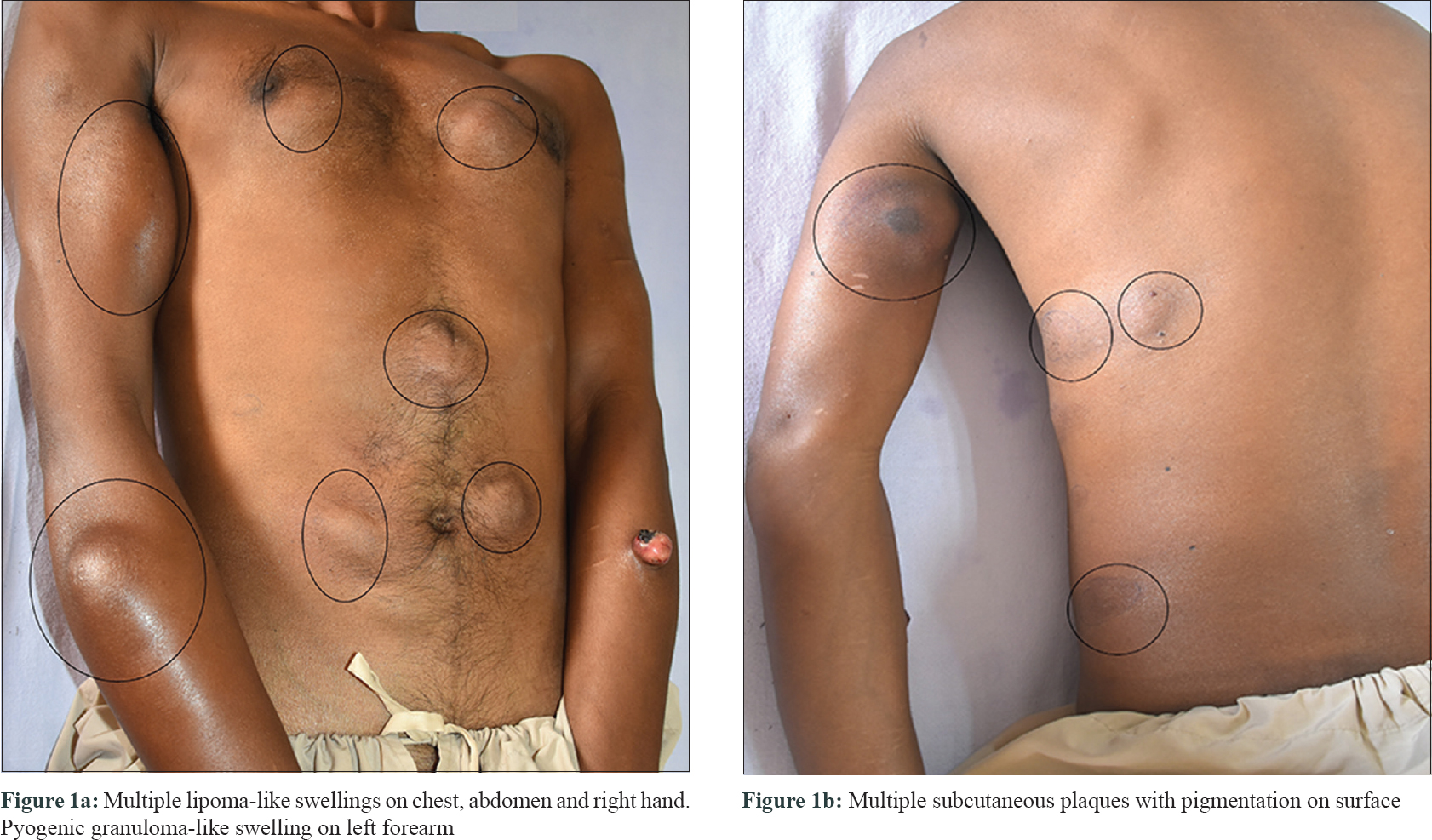
2. Disseminated Cutaneous Rhinosporidiosis
This form is less common and occurs through hematogenous spread, especially in immunocompromised individuals. Lesions may appear on the trunk, limbs, or other areas without involvement of mucosal sites.
3. Primary Cutaneous Rhinosporidiosis
Occurs when the organism directly infects the skin through a break in the epithelium. It may present without any nasal or ocular symptoms.
For Update On Further Important Health Related Topics And Frequently Asked Questions On Health Topics By General Population Please Click On The Link Given Below To Join Our WhatsApp Group –
https://chat.whatsapp.com/Lv3NbcguOBS5ow6X9DpMMA
Lesion Types
- Nodules: Firm, painless nodules that may ulcerate.
- Warty growths: Verrucous lesions resembling viral warts or tuberculosis verrucosa cutis.
- Plaques: Indurated, hyperpigmented plaques mimicking cutaneous leishmaniasis or chromoblastomycosis.
- Polypoid masses: Resemble soft tissue tumors or papillomas.
- Ulcerative lesions: Non-healing ulcers with a granulomatous base.
The lesions are typically painless but may bleed if traumatized. They often persist and slowly enlarge over months or years.
Diagnosis
The diagnosis of cutaneous rhinosporidiosis is primarily histopathological, supported by clinical suspicion and epidemiological background.
1. Clinical Suspicion
Important in endemic areas, especially if the patient has a history of bathing in stagnant water, or presents with chronic, non-resolving skin nodules or plaques.
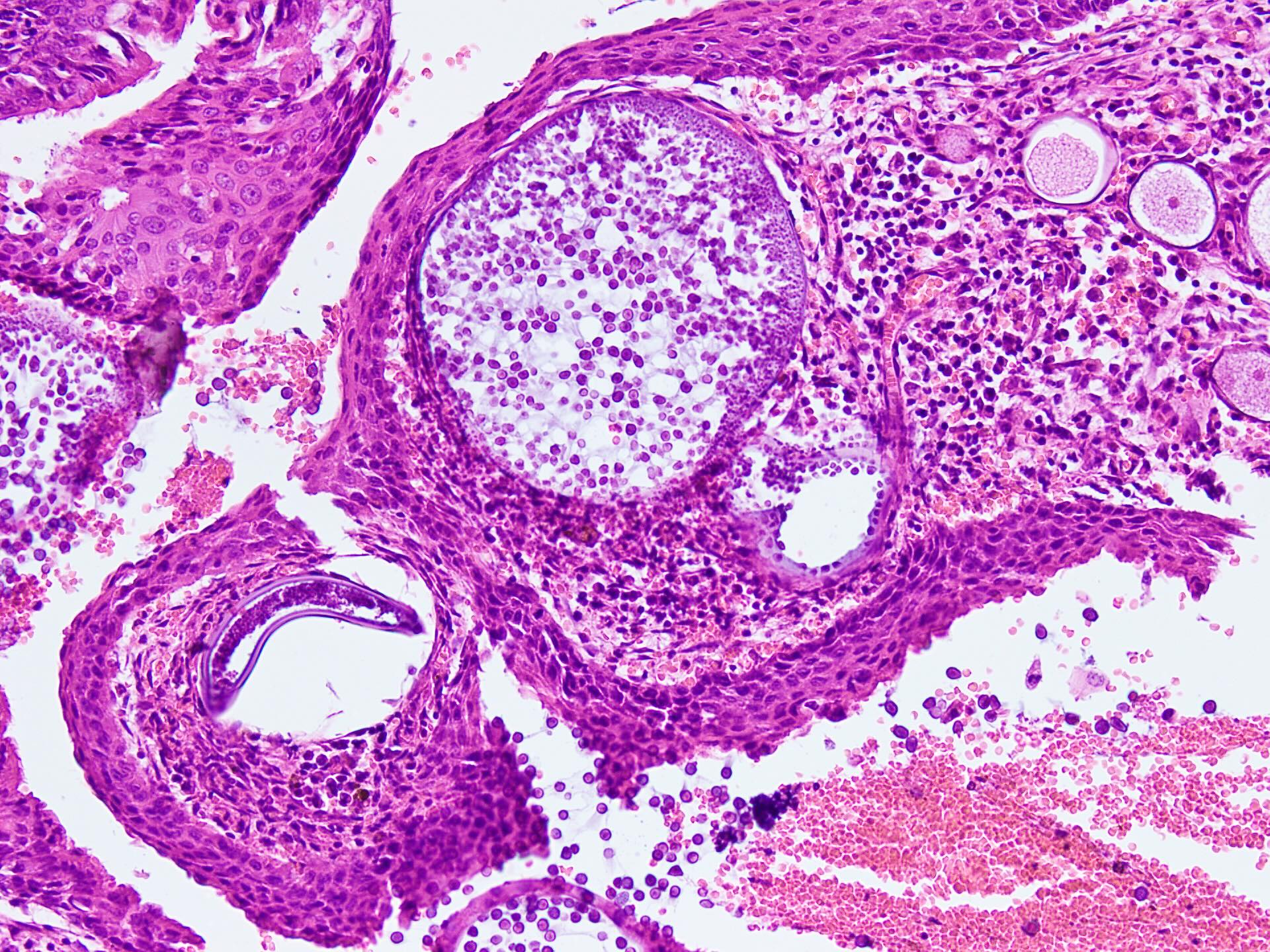
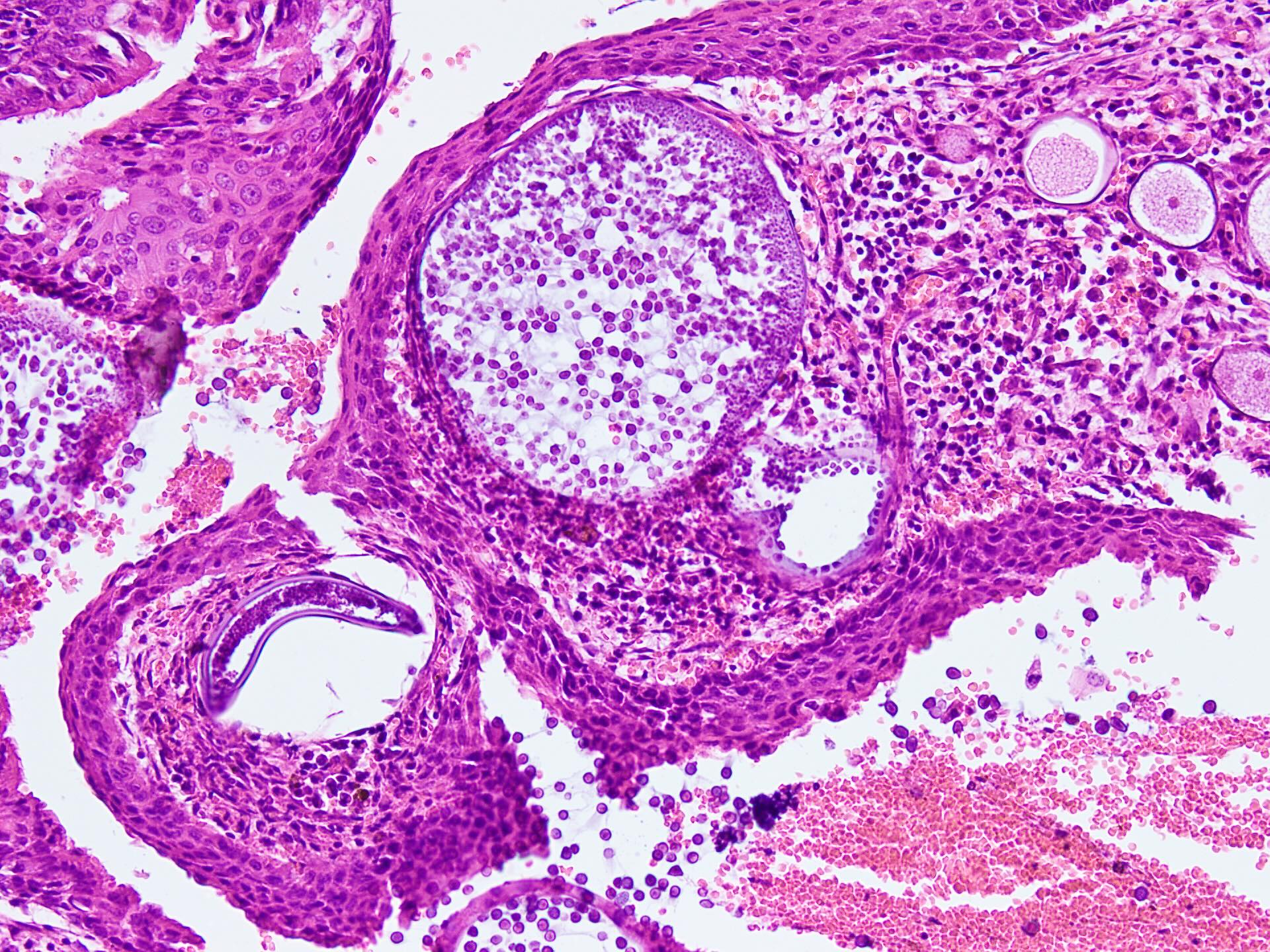
2. Histopathology
This is the gold standard for diagnosis. Key findings include:
- Presence of large, thick-walled sporangia in various stages of development.
- Sporangia containing multiple endospores.
- Dense chronic inflammatory infiltrate with lymphocytes, plasma cells, and macrophages.
- Granulomatous reaction may be present.
3. Fine Needle Aspiration Cytology (FNAC)
FNAC can show large, spherical sporangia with endospores, but may not be definitive.
4. KOH Preparation
Can occasionally reveal the organism, though less sensitive than histopathology.
5. Imaging
Ultrasound or CT may be used to assess deeper lesions or systemic spread but is not specific.
DISCLAIMER-Some patients go to net and directly take treatment from there which can lead to catastrophic consequences-Then- Many people ask then why to read all this text -the reason is that it helps you to understand the pathology better ,you can cooperate with treatment better ,your treating physician is already busy with his patients and he does not have sufficient time to explain you all the things right from ABCD ,so it is always better to have some knowledge of the disease /disorder you are suffering from.
Differential Diagnosis
Due to its varied appearance, cutaneous rhinosporidiosis can mimic many other conditions, such as:
- Cutaneous tuberculosis
- Leprosy
- Chromoblastomycosis
- Cutaneous leishmaniasis
- Verruca vulgaris (common warts)
- Squamous cell carcinoma
- Fungal infections (e.g., sporotrichosis)
A biopsy is often essential to distinguish rhinosporidiosis from these conditions.
Treatment
1. Surgical Excision
- The mainstay of treatment is complete surgical excision of the lesion, followed by electrocauterization of the base to reduce recurrence.
- Care must be taken to remove the entire lesion to prevent seeding of residual spores.
2. Medical Therapy
- Dapsone (100 mg daily) is often used post-operatively to prevent recurrence.
◦ Mechanism: Believed to arrest the maturation of sporangia and promote fibrosis.
◦ Duration: May be continued for several months. - Antifungal or antibacterial agents are ineffective as R. seeberi is not a true fungus or bacterium.
Prognosis and Recurrence
- Prognosis is generally good with proper surgical management.
- However, recurrence is common, especially if excision is incomplete.
- Disseminated and primary cutaneous forms may be more prone to recurrence.
- Long-term follow-up is often necessary.
Prevention
- Avoid bathing in or exposure to stagnant, contaminated water in endemic regions.
- Use protective clothing if exposure is unavoidable.
- Early treatment of mucosal lesions may reduce the risk of cutaneous spread.
Recent Research and Advances
Although R. seeberi has not been successfully cultured in vitro, molecular studies (e.g., PCR and DNA sequencing) have helped clarify its classification. Future developments in genomics and proteomics may lead to:
- Better diagnostic tools (e.g., PCR-based detection)
- New therapeutic targets
- Potential for vaccination or immunomodulatory approaches
However, research remains limited due to the rarity of the disease and challenges in culturing the organism.
Conclusion
Cutaneous rhinosporidiosis is a rare but important dermatological manifestation of Rhinosporidium seeberi infection. Its varied presentation can easily mimic other chronic infections or neoplastic lesions, making histopathological confirmation essential. Though surgical excision remains the cornerstone of treatment, adjunctive therapy with dapsone and preventive measures are crucial in managing recurrence. Increased awareness and timely diagnosis can significantly improve outcomes, especially in endemic regions.
FOR FURTHER INFORMATION IN GREAT DETAIL ON Rhinosporidiosis PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Rhinosporidiosis Pathology Outline PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Rhinosporidiosis Treatment PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
FOR INFORMATION IN GREAT DETAIL ON Rhinosporidiosis Symptoms PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
FOR FURTHER INFORMATION IN GREAT DETAIL ON Rhinosporidiosis Histology PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
FOR FURTHER INFORMATION IN GREAT DETAIL ON Rhinosporidiosis Life Cycle PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
FOR FURTHER INFORMATION IN GREAT DETAIL ON Rhinoscleroma vs Rhinosporidiosis PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
FOR FURTHER INFORMATION IN GREAT DETAIL ON Ocular Rhinosporidiosis PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
FOR FURTHER INFORMATION IN GREAT DETAIL ON Conjunctival Rhinosporidiosis PL CLICK ON THE LINK GIVEN BELOW-It is always better to view links from laptop/desktop rather than mobile phone as they may not be seen from mobile phone. ,in case of technical difficulties you need to copy paste this link in google search. In case if you are viewing this blog from mobile phone you need to click on the three dots on the right upper corner of your mobile screen and ENABLE DESKTOP VERSION.
If any patient has any ENT -Ear nose throat problems and requires any , consultation ,online consultation ,or surgery in clinic of ENT specialist Doctor Dr Sagar Rajkuwar ,he may TAKE APPOINTMENT BY CLICKING ON THE LINK GIVEN BELOW-
Clinic address of ENT SPECIALIST doctor Dr Sagar Rajkuwar-
Prabha ENT clinic, plot no 345,Saigram colony, opposite Indoline furniture Ambad link road ,Ambad ,1 km from Pathardi phata Nashik ,422010 ,Maharashtra, India-Dr Sagar Rajkuwar (MS-ENT), Cel no- 7387590194 , 9892596635




